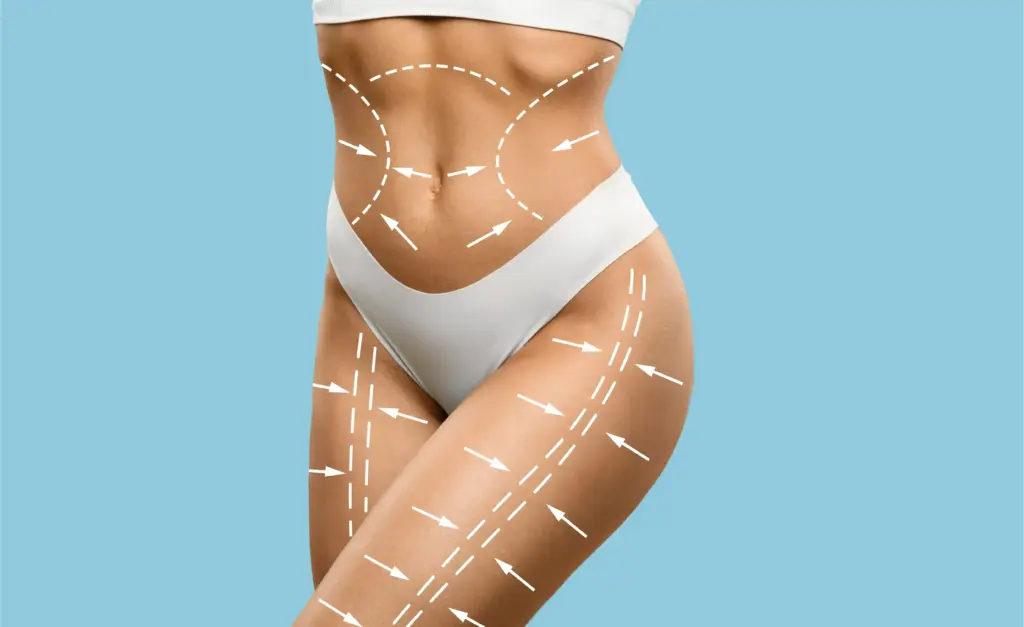
Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
Earlobe keloids are among the most common presentations, often triggered by piercing trauma. These lesions can grow to be massive, sometimes the size of a golf ball, distorting the ear and causing significant social distress. They can be pedunculated (hanging on a stalk) or sessile (broad-based).
Because the earlobe is a non-functional, cosmetic unit, the primary goal is to restore the natural contour. However, the cartilage and skin of the ear are unforgiving. Treatment usually involves a “filet flap” excision, in which the keloid skin is preserved to cover the defect, followed immediately by pressure earrings or steroid injections to reduce the high recurrence rate.

The chest is a high-tension area, making it a prime location for keloid formation (“butterfly keloids”). The constant movement of breathing and the tension of the skin over the sternum stimulate fibroblasts to produce excess collagen. These scars are often painful and tender to the touch.
Chest keloids are notoriously challenging to treat because the tension cannot be eliminated. Surgery is often avoided as a first line because the resulting scar would be under the same stress, leading to a larger recurrence. Aggressive intralesional steroid injections, laser therapy, and cryotherapy are the mainstays of treatment here to flatten the lesion without expanding the wound.

Shoulder keloids often result from vaccinations or acne. Like the chest, the shoulder is a high-motion, high-tension area. Scars here tend to be broad and thick. They can severely restrict the arm range of motion if they contract or become painful.
Treatment often involves a combination of debulking and softening. Pulsed-dye lasers help reduce redness and itching, while injections soften the bulk. If surgery is performed, it is crucial to use extensive undermining (loosening the skin) to relieve tension on the closure, often combined with post-op radiation.
This condition specifically affects the back of the neck and scalp, primarily in men with curly hair. It presents as papules and pustules that merge into large, thick, keloidal plaques. It is caused by chronic inflammation from ingrown hairs and friction from collars.
AKN can lead to permanent hair loss (alopecia) and significant disfigurement. Early treatment focuses on antibiotics and steroids to reduce inflammation. Advanced cases require surgical excision of the entire plaque, often allowing the wound to heal by secondary intention (on its own) to avoid tension and recurrence.

Caesarean sections involve cutting through multiple layers of tissue. The resulting scar can become hypertrophic, forming a thick, red rope just above the pubic hairline. This can be itchy and rub against clothing or underwear, causing functional irritation.
Because there is usually excess skin in this area, surgical revision is highly effective. The old scar is excised, and the new wound is closed with meticulous multi-layer sutures to minimize tension. Post-operative silicone sheeting and taping are critical to ensure the new scar remains flat and fine.
Burns often result in widespread hypertrophic scarring. As these scars mature, they contract (shrink), which can pull on surrounding skin and joints. This leads to contractures, where the limb is frozen in a flexed position, severely limiting function.
Treatment focuses on releasing the contracture. This involves Z-plasty or W-plasty surgeries to lengthen the scar and break up the tension line. In severe cases, skin grafts or flaps are needed to introduce new, healthy tissue into the area to restore the range of motion.


Send us all your questions or requests, and our expert team will assist you.

Keloids can form in the umbilicus (belly button) following piercing or laparoscopic surgery. These can be difficult to treat due to the concave anatomy, which makes compression therapy challenging. They can also become infected easily due to moisture and debris accumulation.
Surgical excision usually involves reshaping the navel. Because of the risk of stenosis (closing up of the belly button), stents or plugs may be used post-surgery to keep the shape while healing. Injections are the preferred first line to shrink the lesion without risking the umbilical structure.
Keloids along the jawline are often sequelae of cystic acne or ingrown hairs (pseudofolliculitis barbae). These can be visually prominent and distort the facial contour. In men, they can interfere with shaving and cause constant irritation.
Treatment must account for the hair follicles. Laser hair removal is often the first step to remove the trigger (ingrown hairs). Once the inflammation subsides, the keloids are treated with injections or excision. Careful alignment of the beard line is essential in surgical reconstruction.
Scars on the upper ear cartilage (helix or tragus) behave differently from earlobe scars. The skin here is thin and adheres directly to the cartilage. Hypertrophy here can be very painful and prone to infection (chondritis).
Treatment involves “coring out” the scar tissue while preserving the underlying cartilage structure. If the cartilage is damaged or infected, it must be debrided. Pressure therapy using custom magnets or clips is essential here, as the cartilage offers a firm backing for compression.
The deltoid region is a classic site for hypertrophic scarring following vaccines (like BCG or smallpox in the past). These scars are often circular or oval and can be atrophic (thin) in the center with a hypertrophic rim.
Treatment focuses on flattening the active rim with steroids or 5-FU. Lasers can be used to blend the texture and color. Surgical excision is approached with caution due to the high tension of the shoulder, often requiring extensive subcutaneous sutures to hold the wound edges together for months.
Traumatic scars often contain embedded debris (asphalt, dirt) from the injury, known as traumatic tattooing. This creates a discolored, irregular scar. The body usually forms a granuloma or hypertrophic scar around this foreign material.
Treatment requires removing the foreign body first. Lasers (Q-switched) can shatter the pigment particles, while CO2 lasers can resurface the irregular texture. Surgical revision is used to excise the worst areas of embedded debris and realign the wound edges for a cleaner linear scar.
Scars crossing the flexor surface of joints (e.g., the inside of the elbow or the back of the knee) are prone to hypertrophy due to constant motion. The stretching stimulates collagen production, while the contraction limits extension.
These are functional emergencies. Treatment involves aggressive physical therapy combined with surgical release. Artificial skin substitutes (dermal matrices) are often used to build a new, flexible dermal layer that allows the joint to move without triggering a new hypertrophic response.


It is strongly discouraged. The fact that you developed a keloid the first time indicates a genetic predisposition. Re-piercing the scar tissue carries an extremely high risk (over 80%) of the keloid returning, often larger than before.
Surgery on the chest is hazardous due to skin tension. We usually start with aggressive injections (steroids + chemotherapy drugs) and laser treatments to flatten it and stop the pain. Surgery is a last resort and must be followed by radiation.
This condition (AKN) is treated by first stopping the inflammation with antibiotics and avoiding short haircuts that irritate the skin. For large lumps, we cut them out and let the wound heal naturally over a few weeks, which yields better results than stitching it closed.
Yes, revision of a C-section scar is very successful. We remove the old, thick scar and carefully sew the new incision in layers to relieve tension on the skin. We also recommend silicone sheets immediately after healing to keep it flat.
The shoulder is a ball-and-socket joint with a massive range of motion. Every time you move your arm, the skin on your shoulder stretches. This constant pulling widens the scar and signals the body to lay down more thick collagen to “reinforce” the area, creating a broad, raised scar.








Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)