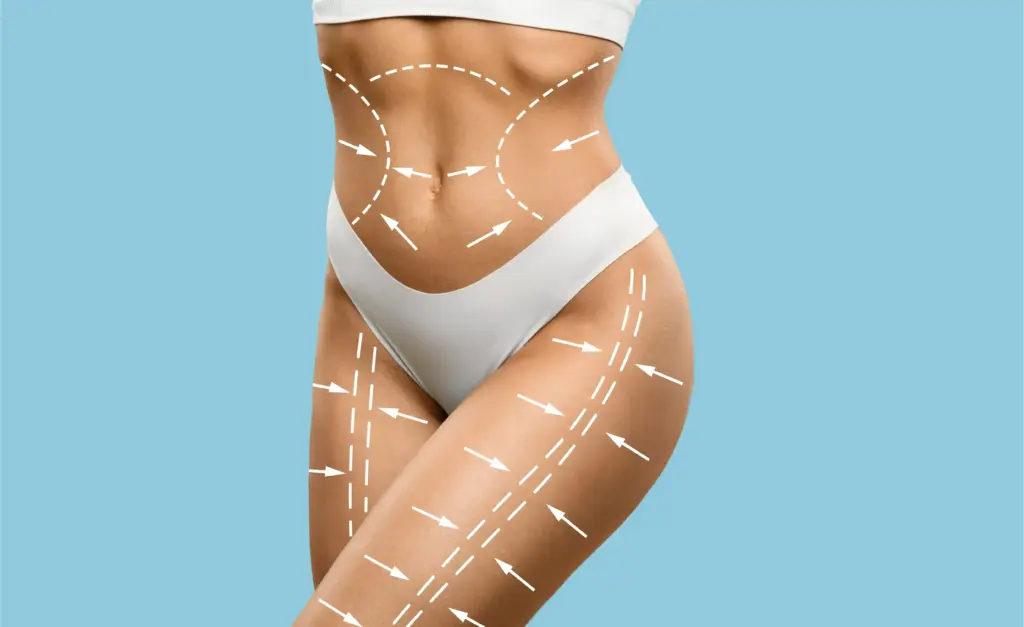
Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
Treating keloid and hypertrophic scars is a specialized area within dermatology and plastic surgery. Normally, scarring helps the body heal, but in these cases, the process goes off track and the body does not stop making collagen when it should. This leads to raised scars that can be painful and bothersome in appearance.
Doctors see these scars as more than just a cosmetic issue—they are actually harmless growths of scar tissue. Treatment involves several steps: stopping the scar-forming cells from multiplying, shrinking the scar, and keeping it from coming back. This field uses both surgery and medications to help restore the skin’s look and function.

Knowing the difference between hypertrophic scars and keloids is key to choosing the right treatment. Hypertrophic scars are raised and red but stay within the area of the original wound. They usually appear soon after an injury and often get flatter on their own, though this can take a long time.
Keloids, on the other hand, grow beyond the original wound and spread into healthy skin. They behave like slow-growing but harmless tumors. Keloids almost never go away by themselves and can keep growing if not treated. Treatments for hypertrophic scars may not work for keloids and can sometimes make them worse.

Both types of scars are caused by an imbalance in the body’s healing process. There is too much inflammation and too much collagen, especially Type III collagen, being made compared to how much is broken down. This leads to a thick, disorganized layer of tissue above the skin.
In keloids, the cells that make scar tissue are extra sensitive to growth signals and do not die off when they should. They keep making collagen long after the wound is healed. Treatments try to break this cycle by slowing down these cells, reducing inflammation, or removing the extra tissue while trying to prevent the scar from coming back.
Injecting steroids like Triamcinolone directly into the scar is the main treatment for both types of scars. This method puts the medicine right where it is needed. The steroid helps by reducing inflammation, shrinking blood vessels to lessen redness, and slowing down the cells that make scar tissue.
This treatment helps soften and flatten the scar over several sessions. It can be used alone for smaller scars or along with surgery to keep the scar from coming back. The dose and how often it is given depend on how thick the scar is and the patient’s skin type, to avoid side effects like light spots or thinning skin.
Cryotherapy treats scars by freezing them with liquid nitrogen. The cold damages the blood vessels in the scar, causing the tissue to die and fall off. This method works best for small, blood-rich keloids and can be done with a probe or a needle.
Cryosurgery is often used together with steroid injections. Freezing the scar causes it to swell, which makes it easier to inject the medicine. This combination helps the steroid spread better, improves results, and makes tough scars respond more to treatment.
Surgical excision means cutting out the scar. But if a keloid is removed by surgery alone, it almost always comes back. That’s why surgery is usually just one part of a bigger treatment plan. The aim is to remove as much of the scar as possible and close the wound without pulling on the skin.
Tension on the skin can cause keloids to form. Surgeons use special ways of closing the wound, like Z-plasty or W-plasty, to change how the tension pulls on the scar. Sometimes, they leave a thin edge of keloid behind to avoid disturbing healthy tissue underneath, which helps prevent new keloids.


Send us all your questions or requests, and our expert team will assist you.

Superficial Radiation Therapy (SRT) is a very effective extra treatment given right after keloid surgery. It destroys the scar-forming cells that are activated by surgery, stopping them from making new collagen and forming another keloid.
This treatment is usually given within 24 to 72 hours after surgery. It only affects the skin and does not go deep into the body, so it is safer. SRT greatly lowers the chance of keloids coming back, often reducing the risk from 90% to less than 10%.
Laser therapy is a non-invasive way to improve how scars look and feel. Pulsed Dye Lasers (PDL) target the blood vessels in the scar, which reduces redness and cuts off oxygen, slowing scar growth. This also helps with itching and burning.
Fractional lasers, which can be either ablative or non-ablative, help reshape scar tissue. They make tiny channels in the scar, breaking up thick collagen and sending heat deep into the skin. This starts a healing process that replaces the tough scar with softer, more normal tissue.
Pressure therapy is a basic, non-surgical treatment, especially for burn scars and earlobe keloids. Keeping steady pressure on the scar cuts down blood flow and oxygen, which slows scar growth. It also helps the scar tissue line up better with the skin.
To work, special garments or clips (for earlobes) need to be worn 12 to 24 hours a day for several months. This takes commitment, but it is a safe, non-invasive way to flatten scars and keep them from coming back after surgery.
Silicone gel sheets are the top choice for non-invasive scar care. They work by keeping the skin hydrated and may help control growth signals in the scar. The silicone forms a barrier that helps the outer skin layer stay moist.
This extra moisture tells the scar-making cells to slow down collagen production. Silicone sheets also protect the scar from rubbing and germs. They are often put on new surgical wounds in high-risk patients to help prevent thick scars from forming.
5-Fluorouracil (5-FU) is a chemotherapy drug that can be injected into scars, often together with steroids. It stops the scar-forming cells from making new DNA, which keeps them from multiplying and making more scar tissue.
This treatment helps when scars do not respond to steroids by themselves. Using 5-FU with steroids works better and has fewer side effects, like thinning skin or spider veins, than using steroids alone. This mix is especially useful for stubborn scars.
New research has led to the use of newer medicines called biologics, such as Interferon, Bleomycin, and Mitomycin C. These drugs work in different ways to slow down cell growth or cause scar cells to die.
These treatments are not used as often as steroids, but they are good options for complicated cases. For example, Bleomycin is used for keloids that are hard to inject or have not responded to other treatments. These medicines are at the forefront of new scar therapies.
The main idea behind treating problem scars is to calm down the skin’s overactive response. This can be done with cooling, pressure, medicines, or covering the scar. The goal is to slow down the scar’s activity.
Doctors try to turn an active, growing, and bothersome scar into one that is stable and not causing symptoms. They usually start with the simplest treatments and only move to surgery or radiation if needed, always focusing on keeping the skin healthy in the long run.


No, generally you should continue taking your cholesterol medication (statins) as prescribed. Controlling your lipid levels helps prevent xanthelasma from recurring. Always confirm medication instructions with your surgeon.
No, you should not wear contact lenses on the day of surgery. You will likely need to wear glasses for the first week or two during recovery to avoid pulling on your eyelids while inserting or removing lenses.
No, keloids are neither contagious nor cancerous. They are benign growths of scar tissue. They cannot spread to other people, and they do not turn into skin cancer, although they can mimic the appearance of some skin cancers, requiring a diagnosis by a doctor.








Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)