Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
Most scar revisions and keloid excisions are performed under local anesthesia. The surgeon injects a mixture of lidocaine and epinephrine directly into and around the scar. This numbs the area entirely and constricts blood vessels to minimize bleeding.
For large or multiple lesions, or for anxious patients, oral sedation or twilight anesthesia may be used. The goal is to ensure the patient is comfortable and pain-free while allowing the surgeon to work with precision. The injection itself can be uncomfortable due to the scar’s density, so slow infiltration and buffering the anesthetic are key techniques.

For keloids, surgeons often employ an “intramarginal” or “fillet” excision. This involves cutting out the core of the keloid but leaving a thin rim of the keloid skin around the edges.
This technique is strategic: it avoids cutting into fresh, unscarred skin, which could trigger a new, larger keloid. It effectively “tricks” the body by failing to stimulate the surrounding healthy fibroblasts. The remaining keloid flap is then folded down to cover the defect.

The golden rule of scar surgery is tension-free closure. Tension on the wound edges signals the body to produce more collagen to “reinforce” the area, leading to a new scar.
Surgeons use extensive undermining (loosening the skin from the underlying tissue) to allow the edges to come together without pulling. They may also use Z-plasties or W-plasties—geometric incision patterns that break up the straight line of the scar and redirect the tension vectors into a more favorable direction.
To maintain the tension-free state, the wound is closed in layers. Deep, dissolvable sutures are placed in the fascia and dermis to hold the strength of the closure. These sutures bear the mechanical load.
The superficial skin is then closed with fine, non-absorbable sutures that merely align the edges. This ensures that even after the skin stitches are removed, the deep stitches continue to hold the wound together, preventing it from stretching or widening during the critical early healing phase.
At the end of the surgery, before the final dressing is applied, the surgeon often injects the wound edges with steroids (Triamcinolone) or 5-FU. This provides an immediate chemical “brake” on the inflammatory process.
This preemptive strike suppresses the fibroblasts right at the moment of injury, reducing the initial signal to overproduce collagen. It sets the biological stage for a calmer healing response.
For cryosurgery, a cryoprobe or needle is inserted into the scar, or a spray is applied. The tissue is frozen to -196°C. The surgeon monitors the “ice ball” formation to ensure the entire scar is treated without freezing the healthy skin.
This is often done in cycles (freeze-thaw-freeze). The patient feels a cold sensation followed by throbbing. A blister typically forms within hours. This is a deliberate, controlled injury to destroy the scar tissue.

Send us all your questions or requests, and our expert team will assist you.

If radiation is part of the plan, the first session typically occurs within 24 hours of surgery. The wound is covered with a lead shield with a cutout matching the incision’s shape.
The SRT machine delivers a precise dose of radiation to the skin surface. The process is painless and takes only a few minutes. It targets the fibroblasts that are rushing to the wound site, sterilizing them so they cannot produce excessive collagen.
The surgical site is dressed with antibiotic ointment and a non-adherent gauze. For earlobe or limb keloids, a pressure dressing is applied immediately. This helps control swelling (hematoma) and provides the first stage of pressure therapy.
Patients are instructed to keep the dressing dry and intact. Pressure is a key component of hemostasis and the long-term success of the procedure.
Post-operative pain is usually manageable. For excision, it feels like a standard cut or bruise. During cryotherapy, the pain can be more intense (throbbing) as the tissue thaws and blisters form.
Pain is managed with over-the-counter analgesics (Tylenol/Ibuprofen) and elevation of the area. Stronger pain medication is rarely needed. Ice packs can be used on the surrounding area (not directly on a graft or frozen site) to reduce inflammation.
Patients are monitored for immediate bleeding or hematoma before discharge. For ear surgeries, the pressure dressing is checked to ensure it isn’t too tight (causing necrosis) or too loose (ineffective).
Discharge instructions are detailed: how to clean the wound, signs of infection to watch for, and the schedule for radiation or suture removal.
Movement creates tension, and tension causes keloids. Patients are strictly instructed to limit movement in the surgical area. For chest or shoulder surgeries, this means no lifting, reaching, or gym activities for at least 2 to 4 weeks.
Minimizing tension on the fresh incision is the most important thing the patient can do to prevent recurrence. The sutures are holding the skin, but excessive movement can rip through the internal repairs.
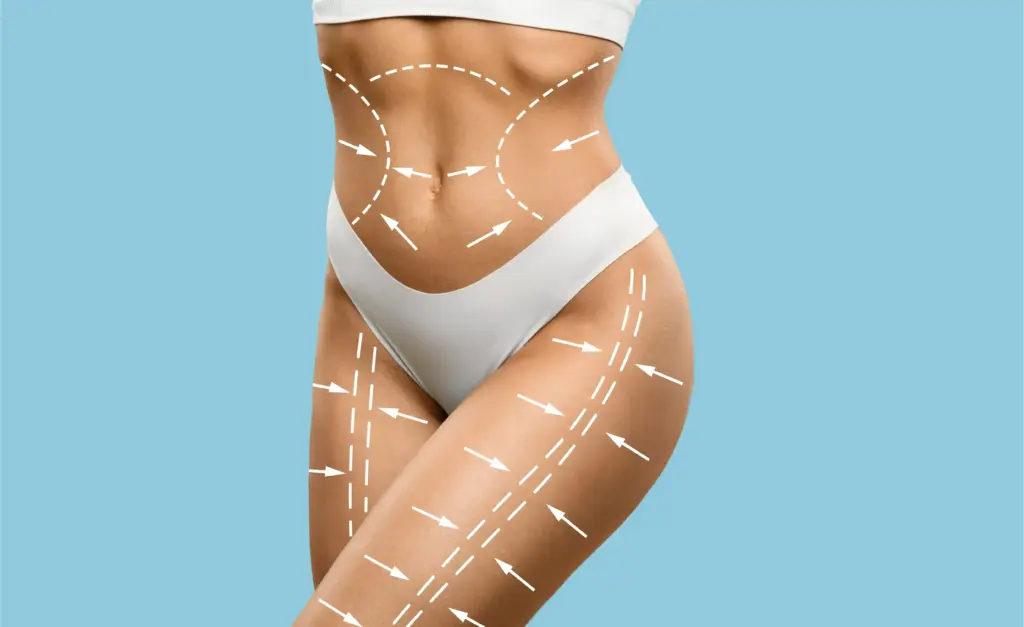
Plastic surgery treatments are highly individualized. The “best” procedure depends on the patient’s anatomy and desired recovery time. Treatments range from non-invasive “lunchtime” procedures to complex, multi-stage reconstructive surgeries.

Yes, for most keloid removals, we use local anesthesia. You will feel a pinch from the numbing shot, then pressure and movement, but no sharp pain. You can talk to the doctor during the procedure.
The radiation treatment itself takes only about 2 to 5 minutes. It is entirely painless, just like getting an X-ray. You will likely need three treatments over three consecutive days after your surgery.
It looks like a large blood blister or a burn blister. It can be dark purple or black. This is normal; it’s the dead scar tissue separating. It will eventually form a scab and fall off, revealing new pink skin underneath.
We usually leave stitches in longer for keloid patients to ensure the wound is strong—typically 10 to 14 days. Sometimes we use dissolving stitches that don’t need to be removed, but we still tape over them to hold the tension.
Usually, you can shower after 24 to 48 hours, but you should not soak the wound (no baths or swimming). Let the water run over it gently and pat it dry. Do not scrub the area. We will give you specific instructions based on your dressing.








Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)