Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The consultation is the foundational step in scar management. It is a comprehensive medical evaluation where the specialist determines the nature of the scar (keloid vs. hypertrophic), the patient’s skin type, and the underlying biological drivers. The physician reviews the history of the scar: how it formed, how fast it is growing, and what treatments have failed in the past.
During this phase, the physician palpates the scar to assess its density, tenderness, and depth. They evaluate the surrounding skin laxity to determine if surgical excision is feasible or if the tension is too high. This diagnostic accuracy is crucial for selecting the right modality from the “reconstructive ladder.”

Scars are rarely just cosmetic concerns; they are often symptomatic. The physician explicitly asks about pain, itching (pruritus), burning, and restriction of movement. These symptoms indicate active inflammation and aggressive fibroblast activity.
Quantifying these symptoms helps in tracking the success of treatment. For example, a reduction in itching is often the first sign that a therapy is working, even before the scar shrinks visually. Addressing these physical symptoms is a primary goal of the intervention.

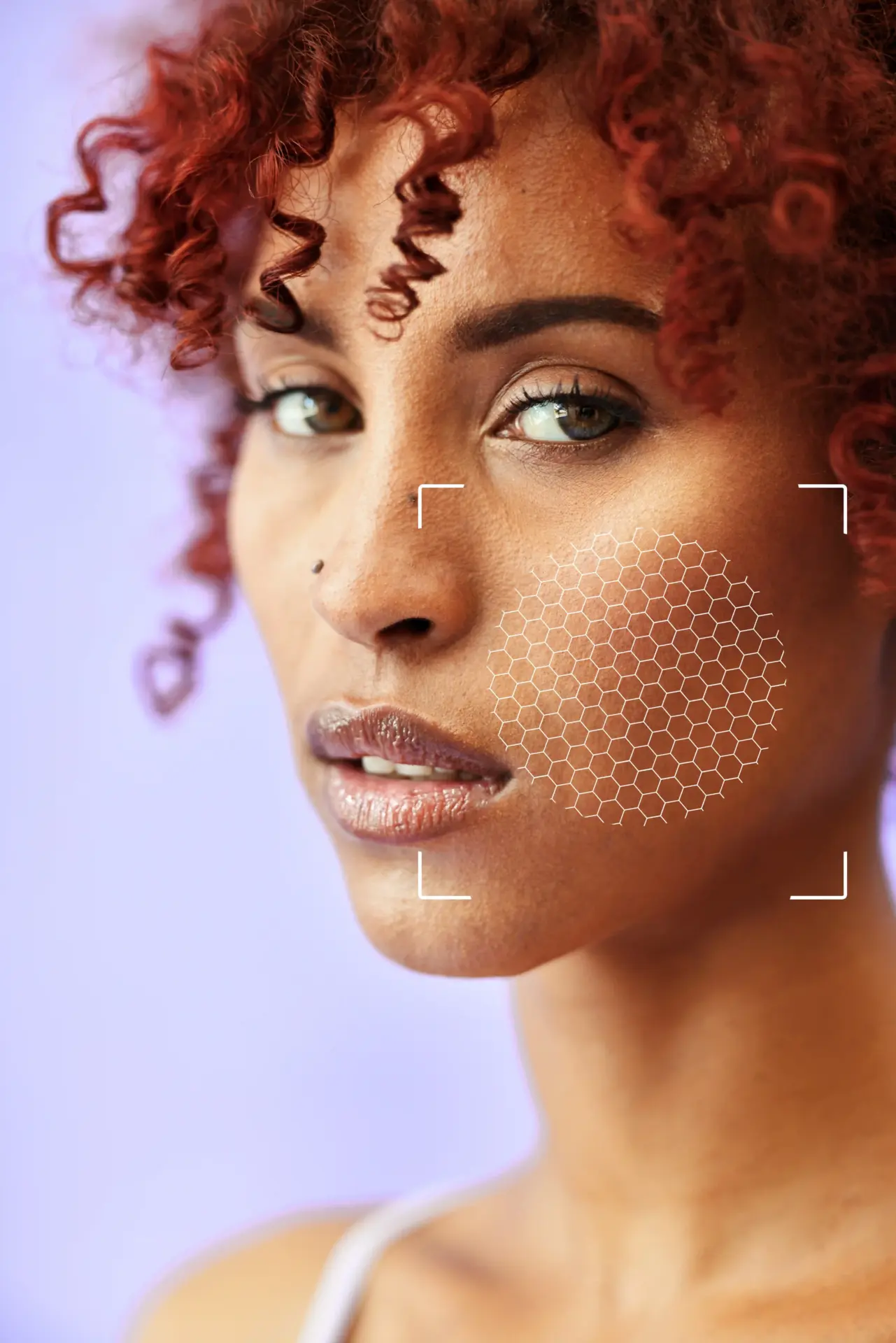
Determining the patient’s Fitzpatrick Skin Type is vital for safety, particularly for laser and radiation therapies. Darker skin types (IV-VI) are more prone to keloid formation and are also at higher risk for pigmentary complications (hypo- or hyperpigmentation) from treatments.
This assessment dictates the energy settings for lasers and the cryotherapy dosing. It also influences the counseling regarding the appearance of the scar after treatment; darker skin may take longer to repigment or may remain lighter than the surrounding tissue.
In some cases, high-frequency ultrasound is used to assess the depth and vascularity of the scar. This imaging can reveal if a keloid extends deeper into the subcutaneous tissue than is visible on the surface.
It also helps objectively measure scar thickness, providing a baseline for monitoring the effectiveness of injection therapies over time. Seeing the vascular flow can guide the use of vascular lasers to target the feeder vessels of the scar.

If the scar is oozing, crusting, or has sinus tracts (tunnels), infection must be ruled out or treated before any revision surgery or injection. Trapped hair follicles or sebaceous cysts within a scar can cause chronic low-grade infection that drives keloid growth.
The physician examines the area for signs of folliculitis or abscess. A course of antibiotics or incision and drainage may be required to “cool down” the lesion before definitive scar treatment can begin.
While most keloids are diagnosed clinically, atypical scars may require a biopsy. If a scar is ulcerated, bleeding, or growing unusually fast, a small sample is taken to rule out malignancies like dermatofibrosarcoma protuberans (DFSP) or squamous cell carcinoma (Marjolin’s ulcer).
This is a safety step to ensure that a cancerous tumor is not mistaken for a benign keloid. The biopsy is performed carefully to avoid stimulating further keloid growth, and is often taken from the center of the lesion.


Send us all your questions or requests, and our expert team will assist you.

A review of systemic health is conducted. Conditions like diabetes, hypertension, or autoimmune disorders can affect wound healing. Patients taking immunosuppressants or anticoagulants require exceptional management.
The physician also assesses the patient’s personal history of scarring. Knowing that a patient developed a keloid from a minor scratch informs the surgeon of the patient’s extreme genetic susceptibility, mandating the most aggressive preventive protocols (such as radiation) immediately after any surgery.
If surgery is planned for a high-risk keloid, a consultation with a radiation oncologist is often scheduled simultaneously. The timing of radiation is critical—it must be delivered within 24 to 72 hours of the surgery.
This logistical coordination ensures that the patient has their radiation appointments scheduled before the surgery. The radiation oncologist maps the treatment field to ensure the beam covers the incision line without exposing underlying organs.
Living with disfiguring or painful scars can cause anxiety and depression. The consultation includes an assessment of the patient’s psychological state and their expectations. Patients must understand that recurrence is a real risk and that “cure” often means a flat, asymptomatic scar, not invisible skin.
Managing expectations prevents post-treatment disappointment. The physician validates the patient’s distress and outlines a realistic timeline, which often involves months of sequential treatments.
Standardized medical photography is essential. Scars change slowly. High-quality photos with consistent lighting and angles provide an objective record of the baseline size, color, and elevation.
These images are used to track progress. Comparing a current photo to the baseline can reveal subtle flattening or paling that might be missed in the day-to-day mirror view, reinforcing the value of the ongoing treatment to the patient.
For patients undergoing surgery or conservative management, compression garment fitting occurs during the preparation phase. Custom pressure earrings or garments are ordered so they are ready to be worn immediately after the procedure.
Patients are educated on the importance of compliance. They need to understand that the pressure device is a medical tool, not an accessory, and must be worn for specific hours to be effective.


Usually, no. An experienced doctor can diagnose a keloid or hypertrophic scar just by looking at it and feeling it. We only do a biopsy if the scar seems unusual, is bleeding, or we suspect it might be something else, like a skin tumor.
Superficial radiation (SRT) is very safe and does not penetrate deep into the body. However, we are cautious with children and very young adults. We weigh the risk of the keloid returning (which is high) against the extremely low theoretical risk of the radiation.
Yes. Smoking reduces oxygen flow to the skin. This delays healing and can actually trigger the body to make more scar tissue as it struggles to close the wound. Stopping smoking is one of the best things you can do to prevent recurrence.
It varies. Most patients need a series of 3 to 6 injections, spaced about 4 to 6 weeks apart, to flatten a scar significantly. We stop when the scar is flat and soft. One injection is rarely enough.
If the scar is causing symptoms such as pain, itching, or restricted movement, insurance often covers the treatment as medically necessary. If it is purely cosmetic (no symptoms), they may not. We will document your symptoms carefully to help with coverage.








Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)