Achalasia maintenance focuses on diet, exercise, and long-term care. Learn how to manage symptoms, protect surgical results, and reduce complication risks.
Send us all your questions or requests, and our expert team will assist you.
Achalasia is a rare disease caused by nerve damage. While there is no cure, focusing on long-term maintenance and care is vital for managing symptoms, supporting healing after treatment, and preventing serious complications like aspiration and the return of dysphagia.
Since primary achalasia is caused by nerve damage, specific diets cannot prevent the disease from starting. However, diet is the most important part of managing symptoms and avoiding complications once the disease has been diagnosed or treated.

Exercise is important for overall health, but movement should be managed carefully to avoid causing discomfort or complicating recovery.

While stress does not cause the disease, it can significantly worsen symptoms by triggering painful muscle spasms. Effective stress management can greatly improve a patient’s comfort.
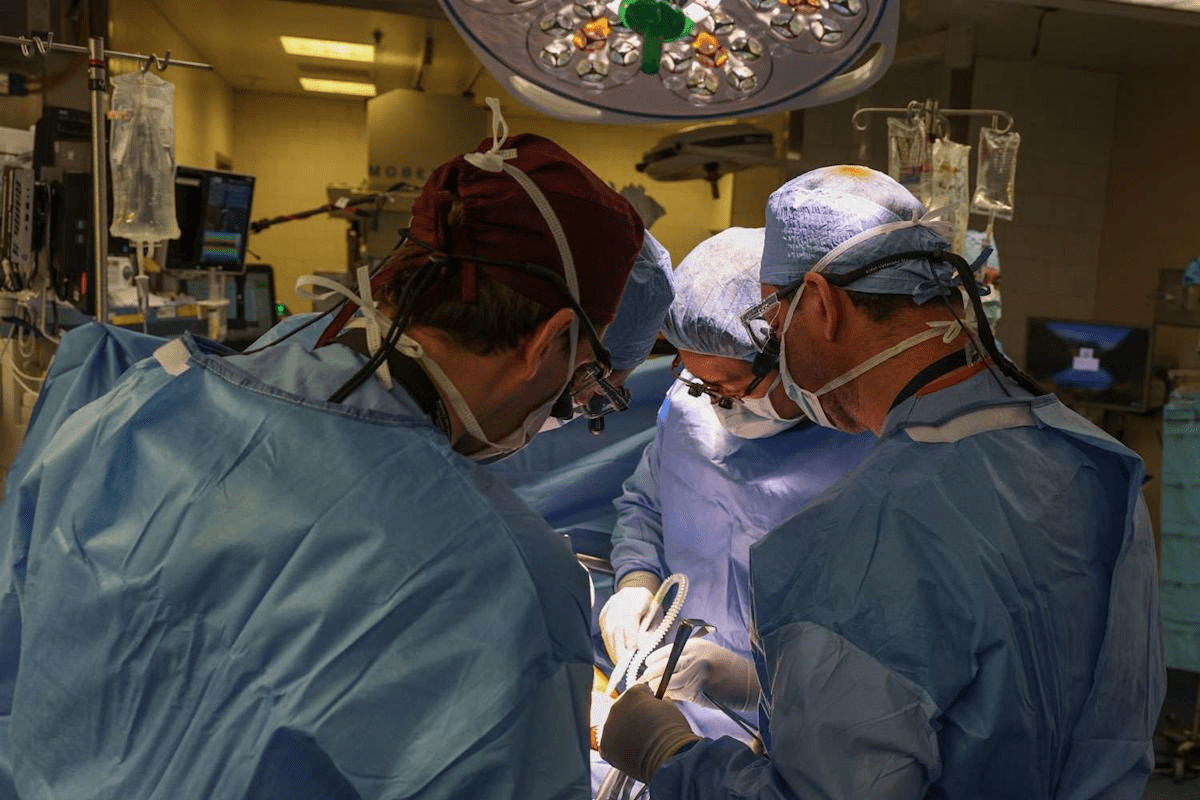
These practices help protect the results of your surgery or procedure and reduce the risk of serious complications.
Regular check-ups are essential for long-term care and preventing serious complications.

Recurrence usually means the return of severe difficulty swallowing because the treated area has tightened up again.

Send us all your questions or requests, and our expert team will assist you.
Since the cause is generally an autoimmune reaction (nerve damage), there are no known lifestyle measures to prevent primary achalasia from starting. Care focuses instead on early diagnosis and proper management to avoid severe complications.
A soft, pureed, or liquid-heavy diet is best. The goal is to choose foods that can easily pass through the obstruction. Patients should avoid dry, dense foods and always use liquids with meals (the “wash-down” technique).
Focus on low to moderate-impact exercises like walking or swimming to maintain overall health. Avoid intense core or strenuous activities that significantly increase abdominal pressure, as this can worsen symptoms like regurgitation.
No, stress is not known to be a cause of the nerve damage that leads to achalasia. However, stress can significantly worsen the symptoms, particularly the muscle spasms that cause intense chest pain.
Key lifestyle changes focus on reducing complication risks: quitting smoking, maintaining a stable, healthy weight, and using a wedge to elevate the head of your bed while sleeping to prevent the dangerous complication of aspiration.


Medical mistakes in hospitals are a big worry. The Institute of Medicine says up to 98,000 deaths annually in the U.S. are due to these

Did you know that nearly 40% of adults worldwide are overweight or obese? Many are looking for effective ways to lose weight. While bariatric surgery
An expert guide on how hernia mesh stays in place. We explore the amazing technology of stitches, tacks, and self-gripping mesh. The choice of technique

It’s estimated that a significant number of patients worldwide are deemed ineligible for hernia surgery due to various health concerns. At our institution, we’ve encountered numerous
Our ultimate guide to hernia treatment success. Discover the amazing 100% curable facts and which repair options are best. With over 700,000 hernia repairs performed

Having a mastectomy can change your life in big ways. Many women worry about how their breasts will look after surgery. Keeping a natural look

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)