Explore achalasia, a rare swallowing disorder. Learn about its symptoms, diagnosis, treatment options, and what to expect from this condition.
Send us all your questions or requests, and our expert team will assist you.
Achalasia is a rare, chronic, and progressive primary motility disorder of the esophagus (the muscular tube connecting the throat to the stomach). It is classified as a neuromuscular disorder because its features stem from the destruction of nerve cells in the esophageal wall.

Achalasia is a rare, insidious, and chronic primary motility disorder of the esophagus. This condition involves a dual neuromuscular pathology: a functional obstruction at the junction of the esophagus and the stomach, coupled with the functional paralysis of the esophageal body. It represents a devastating failure in the coordinated biomechanics required for deglutition (swallowing), leading to severe dysphagia (difficulty swallowing) for both solids and liquids, and subsequent progressive esophageal dilation (megaesophagus).

The term Achalasia is derived from two ancient Greek components, precisely reflecting the primary physiological failure that defines the disease:
When combined, Achalasia literally means “the absence of relaxation” or “failure to relax.”
The underlying cause of achalasia is the selective destruction of the inhibitory neurons within the Auerbach’s (Myenteric) Plexus, a crucial nerve network embedded in the muscular layer of the esophageal wall. These inhibitory neurons release neurotransmitters, primarily Nitric Oxide (NO) and Vasoactive Intestinal Peptide (VIP), which signal the LES muscle to relax. Their destruction leads to two cardinal features:
The diagnosis relies on a multi-modal approach:
Distinguishing achalasia from other esophageal disorders is critical, as treatment pathways are entirely different.
Achalasia is a primary motility disorder involving the loss of inhibitory neurons, requiring treatment that mechanically reduces pressure (like a Myotomy or Dilation). It is emphatically not Gastroesophageal Reflux Disease (GERD) or Reflux Esophagitis. GERD is characterized by a hypotensive (loose) LES allowing acid to flow up into the esophagus, while achalasia involves a hypertonic (tight) LES that prevents food from going down.
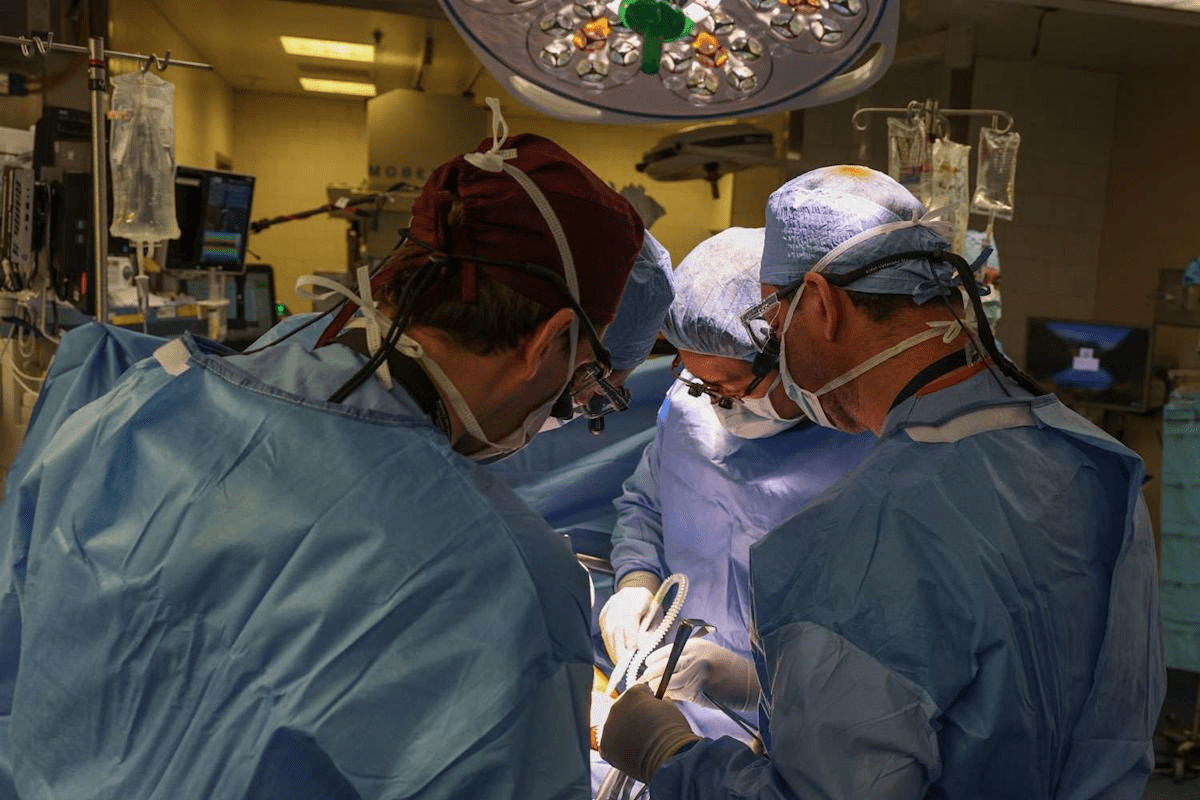
Achalasia management requires collaboration across advanced medical and surgical specialties to ensure the optimal, least invasive treatment is chosen.

The recognition of achalasia subtypes revolutionized treatment planning, as different motor patterns respond better to specific interventions. These types are classified based on the High-Resolution Manometry findings:
The importance of timely and effective treatment for achalasia cannot be overstated, given its severe impact and long-term risks:

Send us all your questions or requests, and our expert team will assist you.
Achalasia is a progressive neuromuscular disorder where the lower esophageal sphincter (LES) fails to relax, and the esophageal body is paralyzed (aperistalsis). A Motility Gastroenterologist is the primary specialist. They utilize High-Resolution Manometry (HRM) to precisely diagnose and classify the disease subtype.
The stasis of food and fluid can lead to several severe complications, including: Megaesophagus (severe widening and tortuosity of the esophagus), Esophagitis (non-acid-related irritation from retained food), Aspiration Pneumonia, significant Weight Loss and malnutrition, and a long-term risk of Esophageal Squamous Cell Carcinoma.
Defined by the Chicago Classification using HRM, the three main types are distinguished by their motor patterns: Type I (Classic), which is marked by a completely inactive esophageal body; Type II (Pressurized), which shows simultaneous pressure increases across the whole esophagus and has the best treatment outcomes; and Type III (Spastic), which is characterized by powerful, premature contractions and is the most difficult to treat.
You should seek a specialist immediately if you experience persistent dysphagia (difficulty swallowing) for both liquids and solids, recurrent regurgitation of undigested food (especially at night), or unexplained weight loss.
Both are esophageal motility disorders. The key distinction is in the LES and the muscle pattern. In Achalasia, the LES is non-relaxing, and the esophageal body is paralyzed (aperistalsis). In DES, the LES relaxation is usually normal, but the esophageal body experiences simultaneous, disorganized, high-amplitude, and non-propulsive contractions (spasms) which cause episodic chest pain and dysphagia.


Medical mistakes in hospitals are a big worry. The Institute of Medicine says up to 98,000 deaths annually in the U.S. are due to these

Did you know that nearly 40% of adults worldwide are overweight or obese? Many are looking for effective ways to lose weight. While bariatric surgery
An expert guide on how hernia mesh stays in place. We explore the amazing technology of stitches, tacks, and self-gripping mesh. The choice of technique

It’s estimated that a significant number of patients worldwide are deemed ineligible for hernia surgery due to various health concerns. At our institution, we’ve encountered numerous
Our ultimate guide to hernia treatment success. Discover the amazing 100% curable facts and which repair options are best. With over 700,000 hernia repairs performed

Having a mastectomy can change your life in big ways. Many women worry about how their breasts will look after surgery. Keeping a natural look

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)