Diagnosing Achalasia requires a Barium Swallow, Endoscopy, & High-Resolution Manometry (HRM). Learn about tests, preparation, and how results classify your condition.
Send us all your questions or requests, and our expert team will assist you.
Diagnosing Achalasia is a step-by-step process that confirms the lack of proper muscle function in the esophagus and rules out other diseases. The diagnostic journey starts with basic screening tests and progresses to advanced procedures like manometry, which is essential for accurately classifying the disease and guiding treatment.

While there are no routine screening tests for the general public, the following procedures are often the first steps taken when a patient presents with classic symptoms like dysphagia (difficulty swallowing) and regurgitation.
The Barium Swallow is typically the first imaging test ordered to evaluate the structure and function of the esophagus.
Upper Endoscopy is a vital procedure used to directly examine the lining of the upper gastrointestinal tract.

If the initial screening tests suggest achalasia, the diagnosis must be confirmed and classified using High-Resolution Manometry.
HRM is the gold standard for diagnosing achalasia, as it directly measures the pressure and coordination of the esophageal muscles.
Proper preparation ensures the safety and accuracy of these diagnostic tests.
Once both the EGD rules out a tumor, and the HRM confirms aperistalsis and elevated IRP, the diagnosis of achalasia is certain.

You need advanced esophageal function testing (HRM) when initial screening tests, like the Barium Swallow, show clear functional problems, but a definitive, classified diagnosis is needed before planning definitive treatment (surgery or dilation). HRM is essential because it is the only test that can distinguish achalasia from other similar motility disorders like Diffuse Esophageal Spasm.

Send us all your questions or requests, and our expert team will assist you.
The primary diagnostic tests are the Barium Swallow (which shows the characteristic “bird’s beak” narrowing), Upper Endoscopy (EGD) (to rule out tumors), and High-Resolution Manometry (HRM), which is the gold standard for measuring muscle function and classifying the disease type.
You must fast (no food or drink) for at least 6 to 8 hours before both procedures. For Endoscopy, you may be asked to follow a clear liquid diet the day before to clear any retained food from the esophagus.
HRM is generally not painful, but it can be uncomfortable. The main discomfort comes from the sensation of the thin catheter being passed through the nose and throat. The procedure is performed without sedation and lasts about 15 to 30 minutes.
High-Resolution Manometry (HRM) is highly accurate (considered the gold standard), providing objective data on muscle failure and sphincter pressure. The Barium Swallow is also highly accurate when showing the classic “bird’s beak” sign.
You need advanced testing like HRM whenever achalasia is suspected based on symptoms and a screening test (like Barium Swallow). HRM is necessary to confirm the specific physiological failures and to determine the Chicago Classification type of achalasia, which directly guides the most effective treatment choice.


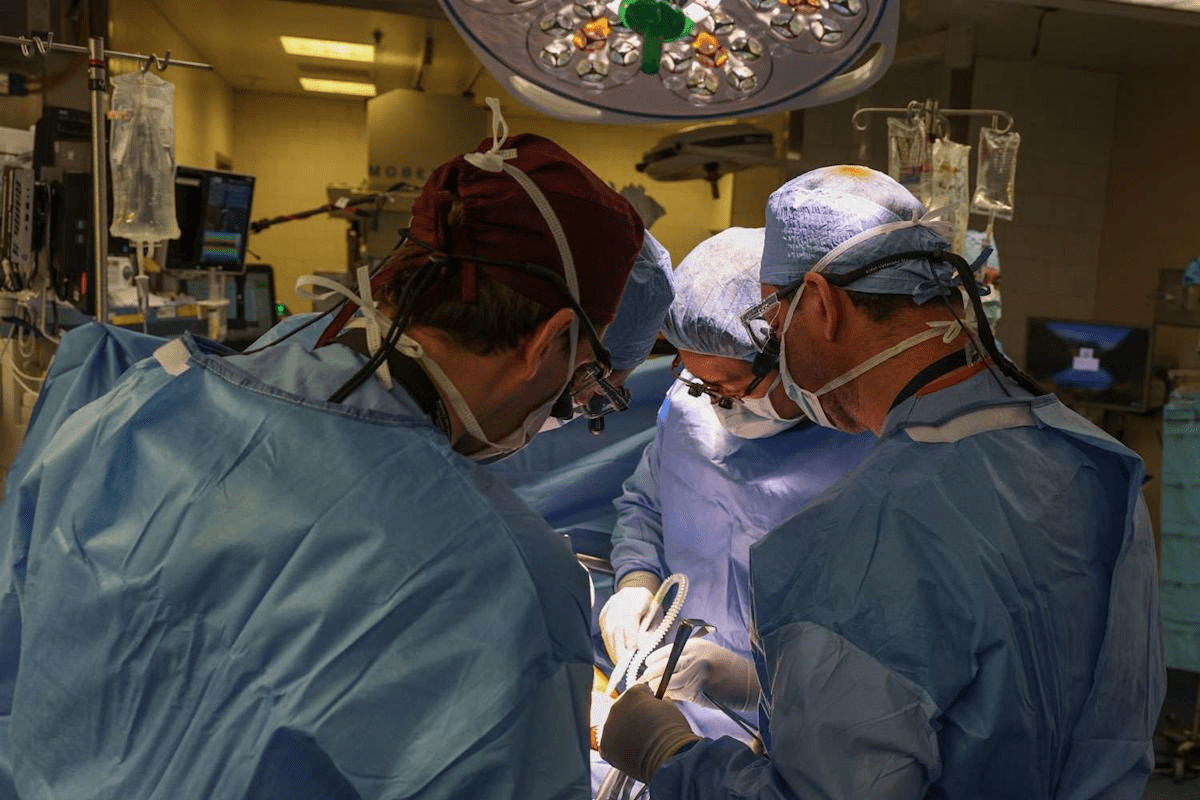
Medical mistakes in hospitals are a big worry. The Institute of Medicine says up to 98,000 deaths annually in the U.S. are due to these

Did you know that nearly 40% of adults worldwide are overweight or obese? Many are looking for effective ways to lose weight. While bariatric surgery
An expert guide on how hernia mesh stays in place. We explore the amazing technology of stitches, tacks, and self-gripping mesh. The choice of technique

It’s estimated that a significant number of patients worldwide are deemed ineligible for hernia surgery due to various health concerns. At our institution, we’ve encountered numerous
Our ultimate guide to hernia treatment success. Discover the amazing 100% curable facts and which repair options are best. With over 700,000 hernia repairs performed

Having a mastectomy can change your life in big ways. Many women worry about how their breasts will look after surgery. Keeping a natural look

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)