Learn about common GI symptoms, from indigestion to viral infections. Discover the causes and how a gastroenterologist can help diagnose and treat them.
Send us all your questions or requests, and our expert team will assist you.
Achalasia is a rare, chronic disorder affecting the esophagus, characterized by the failure of the lower esophageal muscle to relax and a loss of muscle coordination. Recognizing the early, often gradual, symptoms is vital for diagnosis. Understanding the associated risk factors, though largely non-modifiable, helps patients manage their health and seek timely intervention. The main symptoms include progressive difficulty swallowing, regurgitation of food, and chest pain.
The symptoms of achalasia usually develop slowly and worsen over months or even years. The primary feature is that the difficulty swallowing affects both solids and liquids almost equally.

Achalasia is categorized into three types based on the patterns seen during high-resolution manometry (HRM), which can influence the symptoms experienced:

Achalasia itself rarely causes an acute medical emergency, but its complications can be dangerous and require immediate care.
Achalasia is primarily caused by the autoimmune destruction of the nerve cells (myenteric plexus) in the esophagus. Most factors associated with the disease are non-modifiable.
Since the etiology of primary achalasia is believed to be autoimmune/neurological, there are very few established modifiable lifestyle factors that directly cause the condition. However, certain factors may impact the severity of symptoms or the success of treatment.

Generally, there are no significant differences in the primary symptoms or severity of achalasia between men and women.
The total risk of developing primary achalasia is extremely low for the general population, as it is a rare disease. For individuals with progressive, unrelenting difficulty swallowing (dysphagia) that affects both solids and liquids equally, the likelihood of having a motility disorder like achalasia is significantly higher.
Early diagnosis using tests like Barium Swallow (which shows the characteristic “bird’s beak” appearance) and High-Resolution Manometry (HRM) is the only way to accurately quantify the risk and confirm the diagnosis.

Send us all your questions or requests, and our expert team will assist you.
The main warning signs are progressive difficulty swallowing (dysphagia) for both solids and liquids, frequent regurgitation of undigested food and saliva (often without the sour taste of acid reflux), and non-cardiac chest pain due to esophageal muscle spasms.
Individuals between the ages of 30 and 60 are most commonly affected. In specific regions of Central and South America, people exposed to the parasite that causes Chagas Disease are at high risk for developing secondary achalasia.
No. The core symptoms, dysphagia and regurgitation, are similar in both men and women. Any minor differences in symptom intensity are usually related to the subtype of achalasia (like Type III Spastic Achalasia) rather than the patient’s gender.
Lifestyle factors are not known to directly cause primary achalasia. However, smoking can negatively affect healing after surgery, and maintaining a healthy weight is important to prevent symptoms from worsening due to increased abdominal pressure.
No. Primary achalasia is not directly hereditary. It is considered an acquired disorder, likely caused by an autoimmune process. While some autoimmune conditions run in families, achalasia itself does not follow a simple inherited pattern.


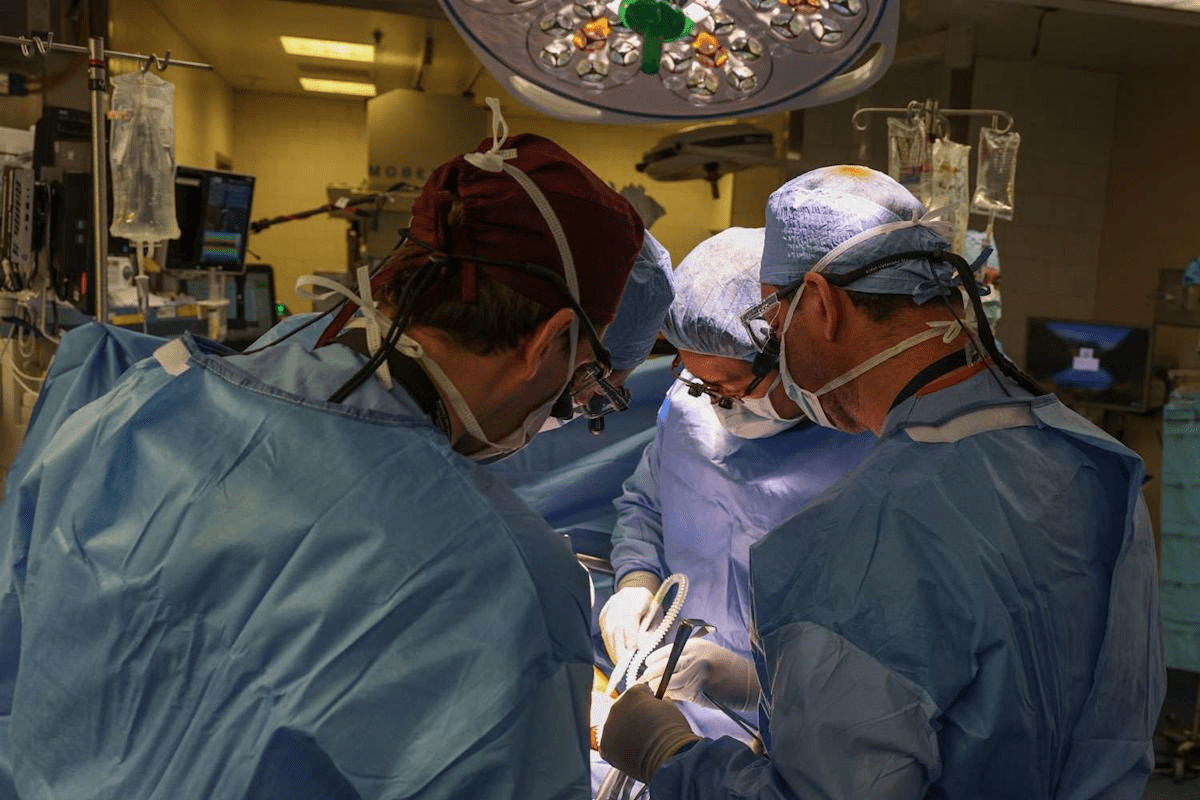
Medical mistakes in hospitals are a big worry. The Institute of Medicine says up to 98,000 deaths annually in the U.S. are due to these

Did you know that nearly 40% of adults worldwide are overweight or obese? Many are looking for effective ways to lose weight. While bariatric surgery
An expert guide on how hernia mesh stays in place. We explore the amazing technology of stitches, tacks, and self-gripping mesh. The choice of technique

It’s estimated that a significant number of patients worldwide are deemed ineligible for hernia surgery due to various health concerns. At our institution, we’ve encountered numerous
Our ultimate guide to hernia treatment success. Discover the amazing 100% curable facts and which repair options are best. With over 700,000 hernia repairs performed

Having a mastectomy can change your life in big ways. Many women worry about how their breasts will look after surgery. Keeping a natural look

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)