Understanding an AD diagnosis. This essential guide explains the 5 key criteria used by doctors to identify Alzheimer’s Disease.
Understanding how to diagnose Alzheimer’s disease has changed a lot. Now, we use NIA-AA criteria that can spot the disease years before symptoms show up.
We’re seeing big changes in how we diagnose Alzheimer’s. Doctors now use both clinical checks and biomarkers to find the disease early. This means we can start treating it sooner.
The NIA-AA guidelines have changed the game. They use new biomarkers to find the disease before symptoms show. This lets doctors give patients the best care possible.
Key Takeaways
- Alzheimer’s disease diagnosis is evolving with the use of advanced biomarkers.
- NIA-AA guidelines provide evidence-based diagnostic criteria.
- Early detection enables earlier intervention opportunities.
- Biomarkers play a critical role in detecting disease pathology.
- Healthcare providers can deliver cutting-edge patient care with the NIA-AA guidelines.
The Evolution of Alzheimer’s Disease Diagnosis
Alzheimer’s disease diagnosis has changed a lot. We now focus on biological signs instead of just symptoms. This change has helped us understand and manage Alzheimer’s better.
From Symptom-Based to Biological Definitions
Before, doctors mainly looked at symptoms and ruled out other causes of dementia. But, new research has led to using biological markers. Biological definitions now include amyloid-beta, tau protein, and markers of brain damage. This makes diagnosing Alzheimer’s more accurate and earlier.
Using biological markers has changed how we diagnose Alzheimer’s. It lets us find the disease years before symptoms appear. This means we can start treatment sooner, which might help more.
Historical Perspective on AD Diagnostic Approaches
Oldly, doctors diagnosed Alzheimer’s based on symptoms like memory loss. They would confirm it by looking at brain tissue after death. They looked for amyloid plaques and neurofibrillary tangles.
Now, we can diagnose Alzheimer’s during a person’s life. We use in vivo biomarkers and imaging. The National Institute on Aging and Alzheimer’s Association (NIA-AA) have helped make these changes.
This move to biological definitions is a big step forward. It opens up new ways to catch Alzheimer’s early. As we learn more, our methods for diagnosing will keep getting better. This gives hope to those affected by Alzheimer’s.
Understanding the NIA-AA Framework for AD Diagnosis
The NIA-AA framework is a big change in how we diagnose Alzheimer’s disease. It’s a joint effort by the National Institute on Aging and the Alzheimer’s Association. Their goal is to make diagnoses more accurate and research more consistent.
What is the National Institute on Aging and Alzheimer’s Association
The National Institute on Aging (NIA) and the Alzheimer’s Association (AA) are key players in Alzheimer’s research. The NIA is part of the National Institutes of Health and focuses on aging and Alzheimer’s. The Alzheimer’s Association works to support those with Alzheimer’s and fund research.
Together, they form the NIA-AA. They aim to deepen our understanding of Alzheimer’s and improve treatments.
The Significance of the 2024 Revised Guidelines
The 2024 guidelines from the NIA-AA are a big step forward in diagnosing Alzheimer’s. They use the latest research and biomarkers to define Alzheimer’s in different stages. This makes it easier to diagnose early and accurately, which is key for treatment and research.
The use of biomarkers is a major breakthrough. Biomarkers are signs of biological processes or how well treatments work. For Alzheimer’s, biomarkers show the presence of amyloid plaques, tau tangles, or brain damage.
The Research Framework Behind the Criteria
The NIA-AA’s criteria are based on the latest science. They focus on biological signs of Alzheimer’s, like biomarkers, not just symptoms. This helps us understand the disease better, even when symptoms aren’t yet present.
The framework also uses a continuum-based approach. It recognizes Alzheimer’s as a disease that progresses in stages, from early to dementia. This model is important for catching the disease early and for designing effective clinical trials.
The Biomarker Revolution in Modern AD Diagnosis
Biomarkers have changed how we diagnose Alzheimer’s disease (AD). They help find the disease early, when it’s easier to treat. Biomarkers are signs in our bodies that show if a disease is present or growing.
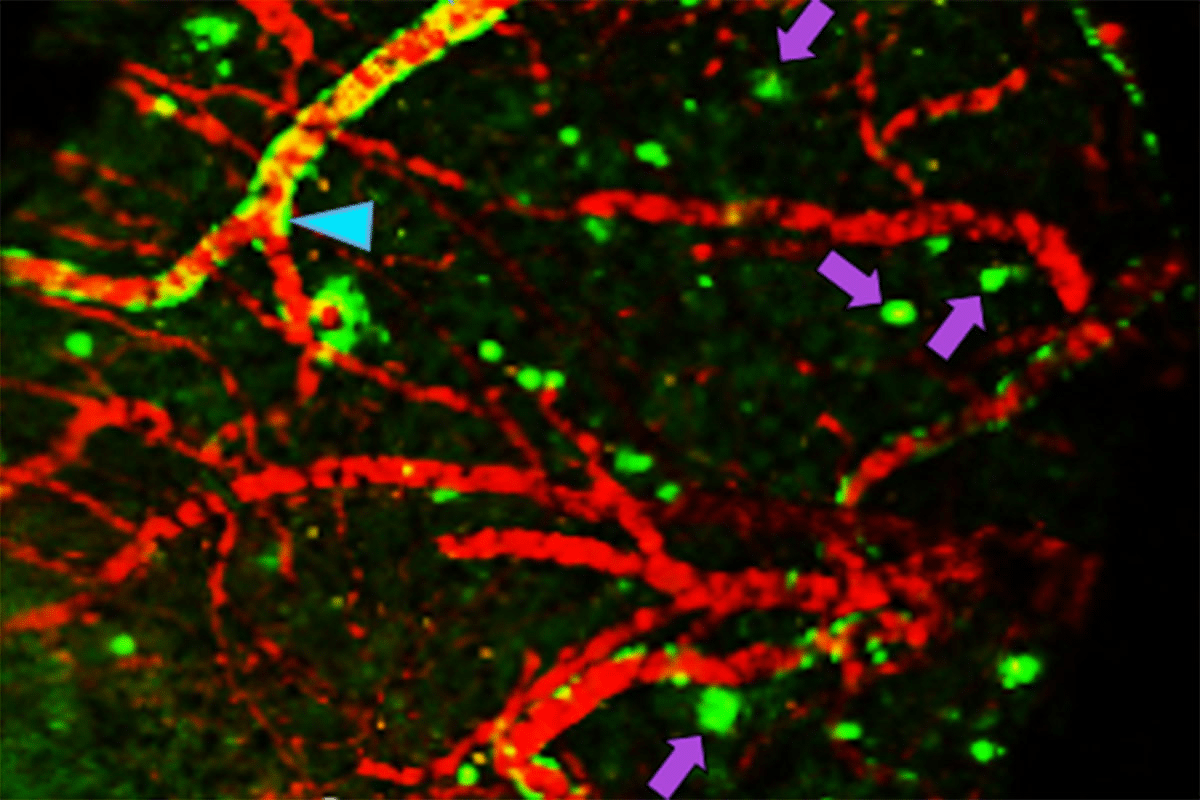
The AT(N) Classification System
The AT(N) system groups biomarkers into three types: Amyloid, Tau, and Neurodegeneration. This helps us understand Alzheimer’s better. It shows how the disease affects our bodies in different ways.
This system gives a detailed view of Alzheimer’s. It shows that the disease is more than just amyloid or tau. It involves many biological processes.
Why Biomarkers Matter for Early Detection
Biomarkers are key for catching AD early. They can spot disease signs years before symptoms show. Finding the disease early lets us start treatments sooner.
With biomarkers, doctors can start early treatments. This might include changes in lifestyle or new medicines. Early detection also helps in research, leading to better treatments.
Detecting Disease Pathology Years Before Symptoms
Biomarkers let us find AD signs years before symptoms show. Studies show amyloid buildup starts long before symptoms appear. This means doctors can diagnose AD before it’s too late.
This early detection opens doors for prevention and new treatments. It highlights the need for more research into Alzheimer’s. The goal is to find effective treatments and improve patient care.
Key Criterion #1: Amyloid Pathology Detection
The NIA-AA guidelines say amyloid pathology is key in diagnosing Alzheimer’s disease. Amyloid pathology is when amyloid-beta peptides build up in the brain. Finding this buildup is vital for accurate diagnosis and tracking the disease.
PET Imaging for Amyloid Detection
PET imaging is a main way to find amyloid pathology. PET imaging uses special tracers that stick to amyloid plaques, showing where amyloid is in the brain. This method gives a clear picture of amyloid levels and is key in research and some clinical settings.
Many studies have shown PET imaging is very good at finding amyloid. But, it has some downsides like being expensive, not always available, and exposing people to radiation.
Cerebrospinal Fluid Aβ42/Aβ40 Ratio
Looking at cerebrospinal fluid (CSF) is another way to spot amyloid pathology. The Aβ42 to Aβ40 peptide ratio in CSF is a key biomarker. A lower ratio means amyloid is building up in the brain.
CSF analysis is more invasive than PET imaging but gives important amyloid information. It’s useful when PET imaging isn’t an option.
Emerging Blood-Based Amyloid Biomarkers
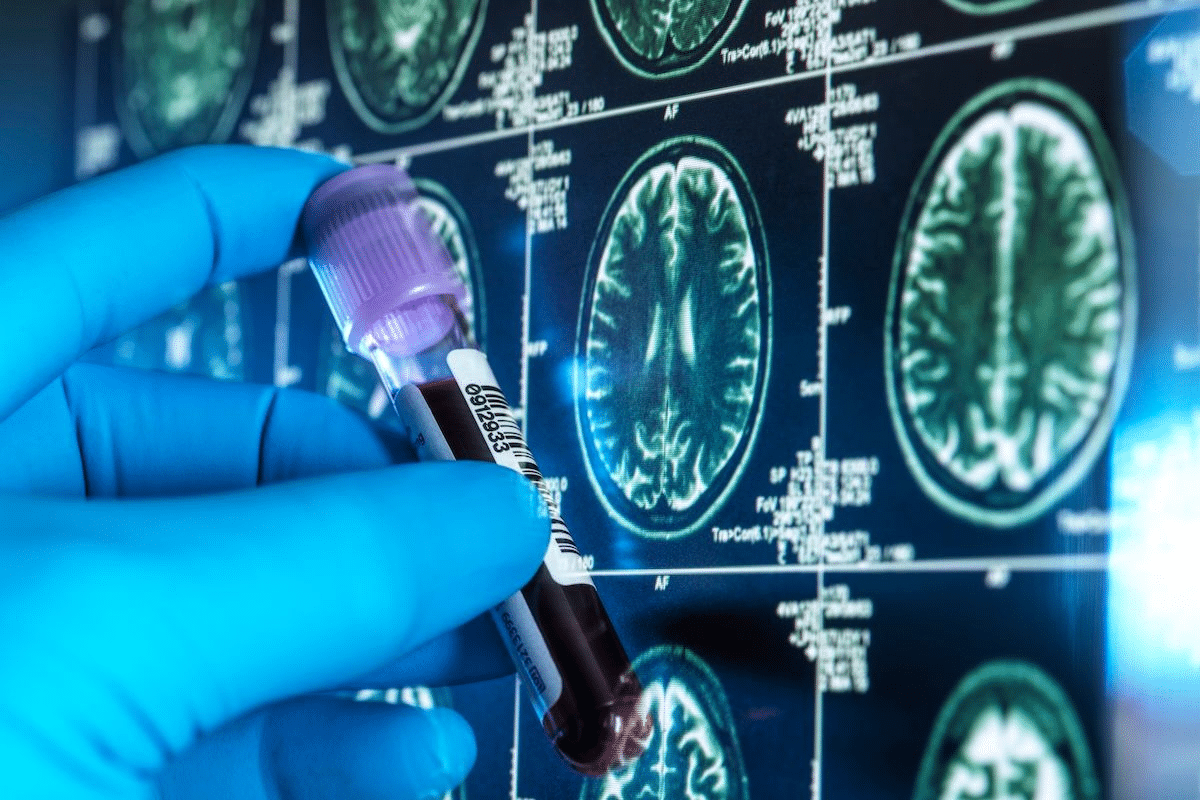
New blood-based biomarkers for amyloid pathology are being developed. These biomarkers could make detecting amyloid easier and less invasive. Studies have shown good results with different blood tests for amyloid-beta peptides.
Even though they’re new, blood-based biomarkers could change how we diagnose Alzheimer’s. They might help us screen more people and catch the disease earlier.
Interpreting Amyloid Biomarker Results
It’s important to understand what amyloid biomarker results mean. Positive results show amyloid buildup, while negative results mean it’s not there. But, these results must be looked at with other diagnostic tools and clinical info to make a correct diagnosis.
Also, knowing the limits and possible errors of each biomarker test is key. As we learn more, making these tests standard and clear guidelines for them will be important.
Key Criterion #2: Tau Pathology Assessment
Tau pathology is key in diagnosing Alzheimer’s disease. It’s vital for understanding the disease and finding new treatments.
“The presence of tau pathology is a hallmark of Alzheimer’s disease, and its assessment can significantly impact our understanding of disease progression,” says Medical Expert, a leading researcher in the field.
Tau PET Imaging Techniques
Tau PET imaging lets us see tau pathology in the brain. This method has changed the field by showing us where tau deposits are. These deposits are linked to Alzheimer’s disease progression.
Tau PET imaging techniques have many benefits. They help track disease progress and check if treatments work. But, this technique is new and not everywhere yet.
CSF Phosphorylated Tau Measurement
Measuring phosphorylated tau in cerebrospinal fluid (CSF) is another important method. It checks for biomarkers linked to Alzheimer’s disease.
The CSF phosphorylated tau measurement helps diagnose Alzheimer’s. High levels of phosphorylated tau often mean AD is present. This test, along with others, makes diagnosing Alzheimer’s more accurate.
Plasma p-tau217 and p-tau181
New plasma biomarkers, p-tau217 and p-tau181, have been developed. They are less invasive than CSF analysis and show promise in diagnosing Alzheimer’s disease.
Plasma p-tau217 and p-tau181 measurements could help detect Alzheimer’s early. More research is needed to confirm their use in clinical settings.
The Relationship Between Tau and Clinical Symptoms
The link between tau pathology and symptoms is complex. Studies show tau is closely tied to cognitive decline in Alzheimer’s disease.
“Understanding the relationship between tau pathology and clinical symptoms is essential for developing effective therapeutic strategies and improving patient outcomes.”
By using tau PET imaging, CSF analysis, and plasma biomarkers, we learn more about Alzheimer’s disease. This knowledge is key for creating targeted treatments and improving diagnosis.
Key Criterion #3: Neurodegeneration Markers
Neurodegeneration markers are key to understanding Alzheimer’s disease. They show how much damage and loss of neurons there is. This is a big part of what makes the disease.
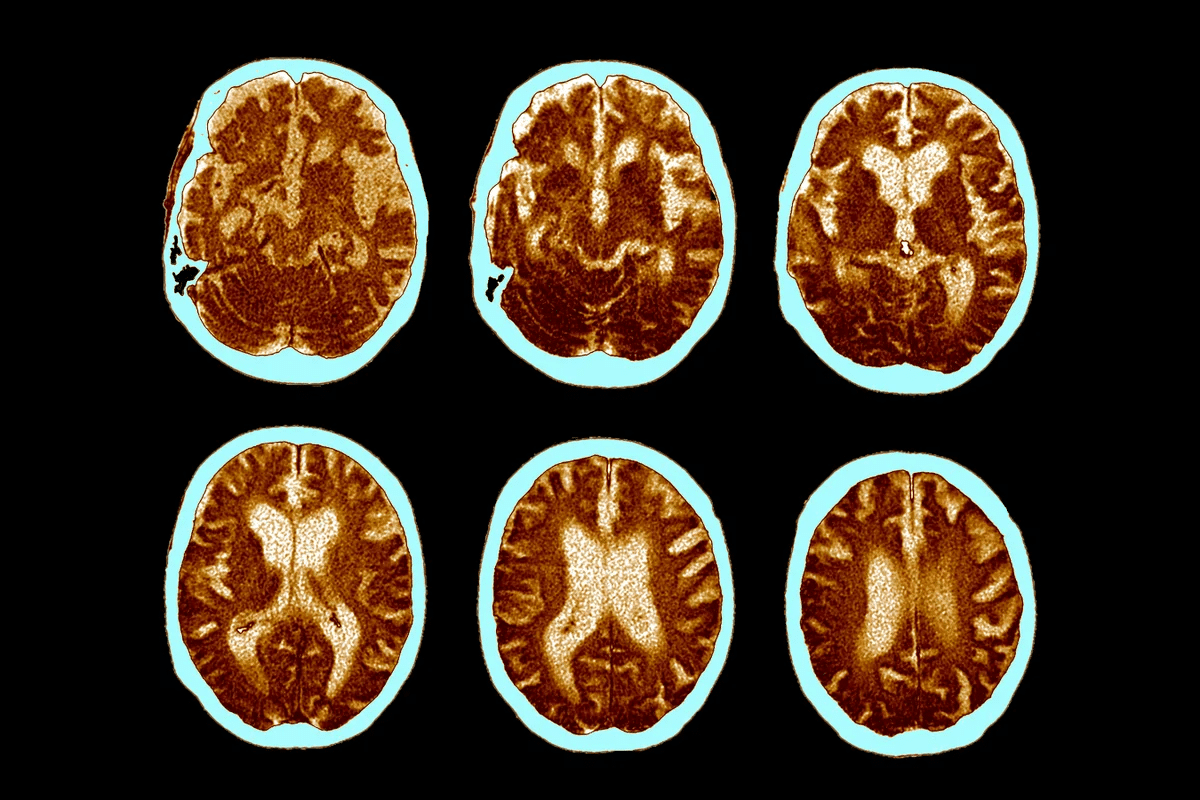
Structural MRI Findings
Structural MRI is a powerful tool for looking at neurodegeneration in Alzheimer’s. It shows changes in the brain, like in the hippocampus and entorhinal cortex. Atrophy in these areas is a big sign of neurodegeneration.
With MRI, we can measure brain region volumes and track changes over time. This is important for diagnosing Alzheimer’s and seeing how it progresses. For example, studies show that hippocampal atrophy is a good marker for Alzheimer’s disease.
FDG-PET Metabolic Patterns
Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) is also important for looking at neurodegeneration. It looks at glucose metabolism in the brain, which is often lower in Alzheimer’s disease areas. Hypometabolism in certain brain regions is a key feature of the disease.
FDG-PET helps find metabolic dysfunction patterns linked to Alzheimer’s. For example, reduced glucose metabolism in the temporoparietal cortex is common in Alzheimer’s patients.
Neurofilament Light Chain and Other Markers
Neurofilament light chain (NfL) is a biomarker of neuronal injury. It can be found in cerebrospinal fluid (CSF) and blood. High levels of NfL mean neurodegeneration and are linked to Alzheimer’s disease. NfL is a promising marker for tracking disease progression and testing treatments.
The Role of Neurodegeneration in Diagnosis
Neurodegeneration markers, like those from structural MRI, FDG-PET, and NfL, are vital for diagnosing Alzheimer’s disease. They give us more information than other biomarkers, like amyloid and tau. This helps us understand how much neuronal damage there is.
By using these markers together, we can make Alzheimer’s disease diagnosis more accurate. This helps us understand how the disease progresses. It also lets healthcare providers create better treatment plans for each patient.
Key Criterion #4: Clinical Staging Across the AD Continuum
The Alzheimer’s Disease continuum is a complex journey from no symptoms to dementia. Understanding this journey is key to diagnosing and managing the disease.
Clinical staging helps doctors identify where a person is in the disease. This allows for tailored care and treatment plans. The stages range from early signs to full dementia.
Preclinical Asymptomatic Disease
Preclinical AD is when people have Alzheimer’s signs but don’t show symptoms. Biomarkers help find this stage early. This way, treatment can start before big cognitive losses happen.
Key characteristics of preclinical AD include:
- Presence of amyloid pathology detected through PET imaging or CSF analysis
- Normal cognitive function
- No noticeable symptoms
Mild Cognitive Impairment Due to AD
Mild Cognitive Impairment (MCI) due to AD is a stage between normal aging and dementia. People with MCI may show cognitive decline but can do daily tasks on their own.
Diagnostic criteria for MCI due to AD include:
- Subjective cognitive complaints
- Objective cognitive impairment
- Preserved functional abilities
- Biomarker evidence of Alzheimer’s pathology
AD Dementia Stages
AD dementia involves cognitive and functional decline. Staging helps doctors predict outcomes and plan care.
The stages of AD dementia are:
- Mild: Noticeable cognitive decline, some assistance required
- Moderate: Significant cognitive decline, daily assistance needed
- Severe: Extensive cognitive and functional impairment, full-time care required
Knowing the clinical stages of AD is key for effective care. Accurate staging lets doctors provide specific support to individuals and their families.
Implementing Effective AD Diagnosis in Clinical Practice
Getting Alzheimer’s disease (AD) diagnosed right is key for patient care. As we learn more about AD, using this knowledge in real-world settings is a big challenge.
Integrating Biomarkers with Clinical Assessment
Using biomarkers with clinical checks is a big step up for AD diagnosis. Tools like amyloid PET imaging and cerebrospinal fluid (CSF) tests give us clues about AD. By mixing these biomarkers with doctor’s evaluations, we get a more accurate diagnosis. For example, a study showed that adding amyloid PET scans to diagnosis plans helped doctors feel more confident and changed treatment for many patients.
Challenges in Accessing Advanced Diagnostic Tools
Even though advanced tools are helpful, they’re hard to get to. They’re expensive, not everywhere, and not standardized. Also, doctors need special training to use them. We need to fix these problems to make sure everyone can get a good AD diagnosis.
Cost-Benefit Considerations in Diagnostic Workup
When we think about testing for AD, we have to think about costs. New tests are more accurate but also pricier. It’s important to weigh the benefits of early detection against the cost of tests. For instance, using biomarkers to spot AD early can save money and resources in the long run.
Ethical Implications of Early Diagnosis
Early AD diagnosis has many ethical sides. It lets us start treatment sooner, but it also worries about patient stress, stigma, and unfair treatment. We must think deeply about these issues when we start early diagnosis. Keeping patient privacy, supporting them well, and teaching about AD are key steps to handle these concerns.
In summary, making AD diagnosis work in real life needs a full plan. We must use biomarkers and clinical checks, tackle access issues, and think about costs and ethics. This way, we can help patients more and make care better for those with AD.
Conclusion: The Future of Alzheimer’s Disease Diagnosis
As we learn more about Alzheimer’s disease, the future of diagnosing it is bright. We’re now using biomarkers and clinical checks to find and treat it early. This is a big step forward.
The NIA-AA guidelines have been key in shaping how we diagnose Alzheimer’s today. They use the latest research and tech to make diagnosis more accurate and tailored to each person.
Looking ahead, we expect more progress in biomarker research. This includes blood tests and new imaging methods. These advancements will help us diagnose Alzheimer’s more accurately and treat it sooner. This will lead to better outcomes for patients.
But, we also need to tackle the challenges of making these tools available to everyone. We must think about the costs and benefits of these technologies. This way, we can make sure everyone gets the care they need, regardless of their situation.
FAQ
What are the NIA-AA guidelines for Alzheimer’s disease diagnosis?
The NIA-AA guidelines are a set of rules for diagnosing Alzheimer’s disease. They were made by the National Institute on Aging and the Alzheimer’s Association. These guidelines help doctors diagnose Alzheimer’s by looking at both clinical signs and biological markers.
What is the significance of biomarkers in Alzheimer’s disease diagnosis?
Biomarkers are key in finding Alzheimer’s disease early. They can spot the disease’s signs years before symptoms show. This early detection helps in diagnosing Alzheimer’s accurately.
What is the AT(N) classification system?
The AT(N) system is a way to classify Alzheimer’s disease. It looks at amyloid, tau, and neurodegeneration. This system gives a clearer view of the disease’s stages and how it progresses.
How are biomarkers used in clinical practice for Alzheimer’s disease diagnosis?
Biomarkers are used with clinical checks to diagnose Alzheimer’s. They help find people with early disease, mild cognitive issues, and full dementia. This approach is more accurate.
What are the different methods for detecting amyloid pathology?
There are several ways to find amyloid pathology. These include PET scans, CSF tests, and blood tests. Each method has its own strengths and weaknesses. The right choice depends on the situation and what’s available.
What is the role of tau pathology assessment in Alzheimer’s disease diagnosis?
Checking for tau pathology is vital in diagnosing Alzheimer’s. It can be done with PET scans, CSF tests, and blood tests. These methods help identify those with tau issues and track the disease’s progress.
What are the different stages of Alzheimer’s disease across the continuum?
Alzheimer’s disease has several stages. These include early disease, mild cognitive issues, and full dementia. Knowing these stages helps in providing the right care and support.
What are the challenges in implementing effective Alzheimer’s disease diagnosis in clinical practice?
There are many challenges in diagnosing Alzheimer’s effectively. These include using biomarkers and clinical checks together, getting access to advanced tools, and considering costs. Ethical issues also play a role in diagnosing and managing the disease.
What is the future of Alzheimer’s disease diagnosis?
The future of diagnosing Alzheimer’s looks promising. Advances in biomarkers, imaging, and clinical tools are expected. These will lead to earlier and more accurate diagnoses, improving patient care and treatment options.
References
National Center for Biotechnology Information. Alzheimer’s Diagnosis: Key NIA-AA Criteria Explained. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5958625/





