Cardiac amyloidosis is a serious condition where abnormal amyloid protein builds up in the heart muscle. This buildup messes with the heart’s structure and how it works. It’s a big worry because it’s often missed and can look like common heart failure.amyloidosis heart symptomsCardiomyopathy Heart Muscle Disease
If you’re feeling really tired, having trouble breathing, or noticing your heart beating fast, it might be a sign. These symptoms, along with carpal tunnel syndrome, could mean your heart is being quietly damaged. Studies show that more people are affected than we thought.
It’s important to know the signs of cardiac amyloidosis to get help quickly. We’ll look at the main symptoms to help you spot them and get the care you need.
Key Takeaways
- Cardiac amyloidosis is a serious and underdiagnosed condition.
- It involves the accumulation of abnormal protein deposits in the heart muscle.
- Symptoms can include unexplained fatigue, shortness of breath, and heart palpitations.
- Carpal tunnel syndrome can be associated with cardiac amyloidosis.
- Early recognition of symptoms is key for timely medical help.
Understanding Cardiac Amyloidosis and Its Types
Amyloid deposits in the heart are what define cardiac amyloidosis. It’s a serious condition often missed by doctors. We’ll look into what it is, its types, and how it affects people differently.
What Is Cardiac Amyloidosis?
Cardiac amyloidosis happens when abnormal proteins, called amyloid, build up in the heart. This buildup makes the heart walls stiff. It’s harder for the heart to fill with blood and pump well.
This condition can really lower your quality of life. Symptoms include shortness of breath, feeling tired, and swelling in the legs and feet.
The Three Main Types of Cardiac Amyloidosis
There are three main types of cardiac amyloidosis, each with its own traits:
- Immunoglobulin Light-Chain Amyloidosis (AL Amyloidosis): This type is linked to plasma cell dyscrasias. It’s caused by abnormal light chain proteins.
- Hereditary Transthyretin Amyloidosis (ATTRm Amyloidosis): It’s caused by genetic mutations in the transthyretin gene. This leads to abnormal transthyretin protein production.
- Wild-Type Transthyretin Amyloidosis (ATTRwt Amyloidosis): This form happens when normal transthyretin protein misfolds. It usually affects older men.
Prevalence and Epidemiology
Recent studies show cardiac amyloidosis is more common than thought. It affects certain groups more.
|
Type of Amyloidosis |
Prevalence |
Commonly Affected Population |
|---|---|---|
|
AL Amyloidosis |
Approximately 3,000 new cases annually in the US |
Individuals with plasma cell dyscrasias |
|
ATTRm Amyloidosis |
Varies by genetic mutation prevalence |
Families with hereditary transthyretin amyloidosis |
|
ATTRwt Amyloidosis |
Increasingly recognized in older adults, specially men |
Older men, typically over 65 years |
Knowing how common cardiac amyloidosis is helps with early diagnosis and treatment.
Risk Factors and Causes of Cardiac Amyloidosis
It’s important to know what causes cardiac amyloidosis to catch it early. This condition happens when amyloid proteins build up in the heart. This buildup can lead to a stiff heart that can’t pump well.
Age-Related Risk Factors
Getting older increases the chance of getting cardiac amyloidosis. Most people with this condition are over 60. As we get older, our bodies are more likely to misfold amyloid proteins, which is a big part of this condition.
Genetic Predisposition
Some people are more likely to get cardiac amyloidosis because of their genes. For example, some people have a gene mutation that leads to hereditary transthyretin amyloidosis (hATTR). Genetic tests can spot these risks early, helping doctors keep a close eye on them.
Underlying Health Conditions
Having certain health issues can also raise the risk of cardiac amyloidosis. For example, conditions like multiple myeloma can cause abnormal proteins to build up in the heart. Managing these conditions well is key to preventing cardiac amyloidosis.
Protein Misfolding Mechanisms
Protein misfolding is a big part of how cardiac amyloidosis starts. Proteins usually fold into shapes that let them work right. But when they don’t, they can clump together and build up in the heart. Learning about how proteins misfold helps doctors find new ways to treat it.
Knowing the risks and causes of cardiac amyloidosis helps doctors catch it early. This is important for improving how well patients do with this condition.
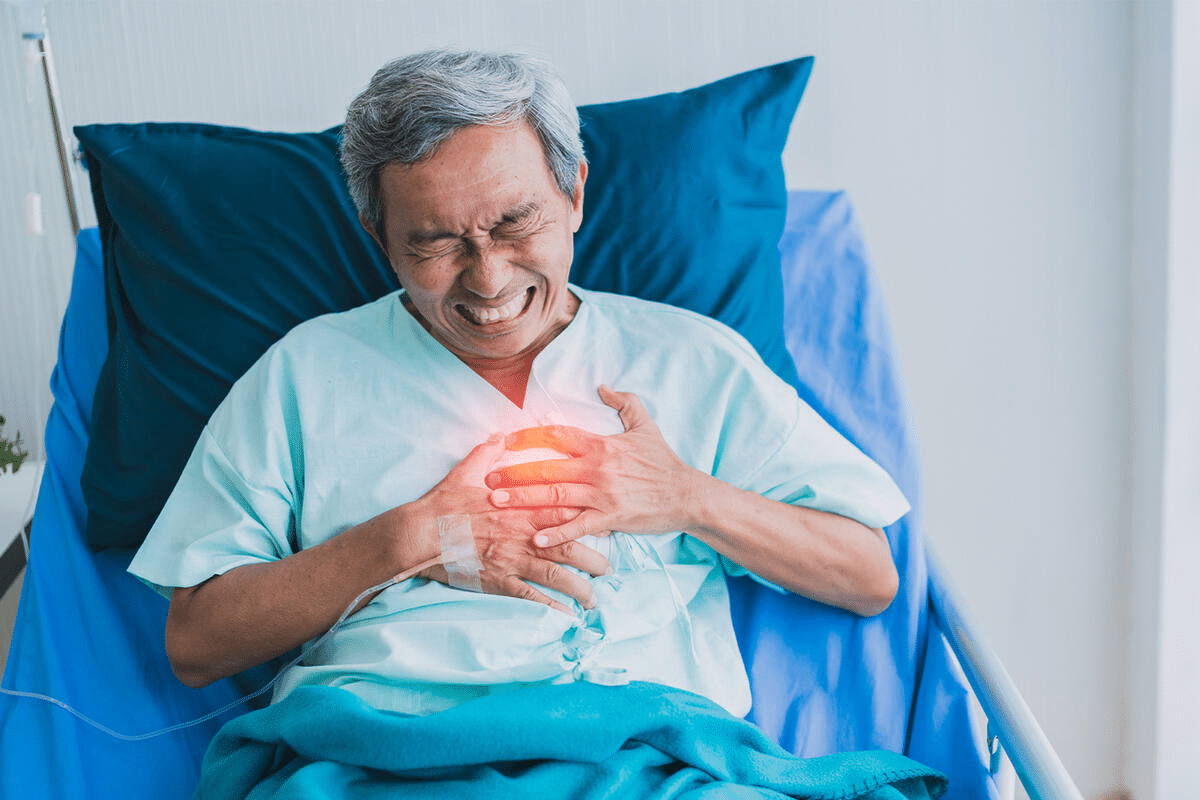
Recognizing Amyloidosis Heart Symptoms: Why Early Detection Matters
Finding amyloidosis heart symptoms early can greatly help patients. Cardiac amyloidosis happens when abnormal proteins build up in the heart. This can lead to serious heart problems.
The Progressive Nature of Cardiac Amyloidosis
Cardiac amyloidosis gets worse over time. At first, symptoms might be mild. But as it gets worse, they can become more serious.
Early signs include progressive dyspnea on exertion and fatigue. These symptoms can be hard to spot because they can look like other health issues.
As the disease gets worse, the heart struggles more. This leads to even more severe symptoms. Knowing about cardiac amyloid symptoms and how they get worse is key to catching it early.
Challenges in Diagnosis
Finding cardiac amyloidosis can be tough. Its symptoms are not clear-cut and can look like other heart problems. Doctors need to be extra careful, looking for signs in people at risk.
Spotting it early is vital for the right treatment. We need to know the symptoms of cardiac amyloidosis and act fast if we see them.
When to Consult a Healthcare Provider
If you’re feeling short of breath, tired all the time, or have swelling, see a doctor. Early checks can help catch and treat cardiac amyloidosis before it gets worse.
Stay alert to amyloidosis heart symptoms and get help if they don’t go away or get worse. A doctor can check you out and figure out the best course of action.
Symptom 1: Shortness of Breath (Dyspnea) and Decreased Exercise Tolerance
Shortness of breath, or dyspnea, is a key symptom of cardiac amyloidosis. It happens because the heart can’t pump blood well. This makes it hard for patients to do daily tasks and live independently.
How Amyloid Deposits Affect Breathing
Amyloid deposits make the heart muscle stiff. This makes it hard for the heart to pump blood. The heart gets stiff, or restrictive cardiomyopathy, and can’t handle extra work. Fluid builds up in the lungs, causing shortness of breath.
Progressive Nature of Activity Limitations
As cardiac amyloidosis gets worse, the heart can’t handle physical demands. At first, patients might only feel short of breath when they’re very active. But as time goes on, even small activities can be hard. This shows the disease is getting worse.
Distinguishing from Other Causes of Dyspnea
Dyspnea can mean different things, like heart failure or COPD. But in cardiac amyloidosis, it often comes with fatigue and swelling. To find the cause, doctors need to do a thorough check-up.
|
Symptom |
Cardiac Amyloidosis |
Other Conditions |
|---|---|---|
|
Dyspnea |
Often accompanied by fatigue and swelling |
May be isolated or accompanied by different symptoms |
|
Exercise Tolerance |
Progressively limited |
Varies depending on the condition |
Impact on Daily Activities and Quality of Life
Shortness of breath and less ability to exercise really affect daily life. Simple tasks become hard, and patients might need help. This loss of independence can hurt mental health and overall well-being. Early diagnosis and treatment are key.
Understanding dyspnea in cardiac amyloidosis helps doctors create better treatment plans. This improves patients’ symptoms and quality of life.
Symptom 2: Persistent Fatigue and Weakness
Cardiac amyloidosis often shows up as persistent fatigue and weakness. This greatly affects patients’ quality of life. It’s not just feeling tired; it’s a deep, ongoing lack of energy that makes daily tasks hard.
The Connection Between Heart Function and Energy Levels
The heart pumps blood all over the body, giving oxygen and nutrients to tissues. In cardiac amyloidosis, amyloid proteins build up, messing with the heart’s work. This leads to less blood flow, causing tissues and muscles to get less oxygen and nutrients. This results in feeling tired and weak.
Differentiating Amyloidosis Fatigue from Other Conditions
Fatigue can mean many things, making it hard to spot cardiac amyloidosis just by feeling tired. But, the fatigue in cardiac amyloidosis is deep and lasts a long time, not going away with rest. We must look at other signs and tests to really know if someone has cardiac amyloidosis.
Management Strategies for Energy Conservation
Handling fatigue means making lifestyle changes and sometimes getting medical help. Energy conservation is important; this means doing things at a slower pace, taking breaks, and focusing on the most important tasks first. Also, gentle exercises, like cardiac rehab, can boost heart health without pushing too hard.
Symptom 3: Swelling (Edema) in the Extremities
Edema, or swelling, in the extremities is a key symptom of cardiac amyloidosis. It’s important to know why it happens, where it shows up, and how to handle it.
Why Fluid Retention Occurs in Cardiac Amyloidosis
Fluid retention in cardiac amyloidosis happens because the heart can’t pump blood well. Amyloid deposits in the heart make it less efficient. This leads to fluid buildup, mainly in the limbs.
The Mechanism Behind Edema: Amyloid makes the heart walls stiff. This makes it hard for the heart to fill with blood between beats. The veins get more pressure, causing fluid to leak into tissues, leading to swelling.
Common Areas Affected by Edema
Edema often hits the legs, ankles, and feet in cardiac amyloidosis. But it can also show up in hands and face, depending on how bad the disease is.
- Legs: Swelling often starts in the lower legs.
- Ankles and Feet: These areas are prone to swelling due to gravity.
- Hands: Less common but can occur, if the patient is bedridden.
Managing Swelling Symptoms
Managing edema needs lifestyle changes, medical treatments, and watching the symptoms. Elevating the affected limbs helps by pushing fluid back to the heart.
Other ways to manage include:
- Using diuretics to help the body get rid of extra fluid.
- Limiting salt intake to reduce fluid retention.
- Doing gentle exercises, as advised by a healthcare provider, to boost circulation.
Symptom 4: Irregular Heartbeat and Palpitations
Irregular heartbeat and palpitations are signs of amyloid deposits in the heart. These symptoms happen when amyloid fibrils invade the heart tissue. This invasion disrupts the heart’s normal function.
Arrhythmias Associated with Cardiac Amyloidosis
Cardiac amyloidosis can cause different arrhythmias. These include atrial fibrillation, ventricular tachycardia, and heart block. These arrhythmias happen because amyloid deposits mess with the heart’s electrical system.
We will discuss the types of arrhythmias and their implications for patients with cardiac amyloidosis.
Potential Complications of Heart Rhythm Disturbances
Arrhythmias from cardiac amyloidosis can lead to serious problems. These include stroke, heart failure, and sudden cardiac death. It’s important to understand these risks to manage the condition well.
A detailed overview of the possible complications is provided in the following table:
|
Complication |
Description |
Risk Factors |
|---|---|---|
|
Stroke |
Occurs when the blood supply to the brain is interrupted, potentially due to blood clots formed in the heart. |
Atrial fibrillation, history of stroke |
|
Heart Failure |
A condition where the heart is unable to pump enough blood to meet the body’s needs. |
Arrhythmias, amyloid burden |
|
Sudden Cardiac Death |
An unexpected death caused by a cardiac condition, often due to severe arrhythmias. |
Ventricular tachycardia, heart block |
Treatment Approaches for Cardiac Arrhythmias
Treating arrhythmias in cardiac amyloidosis involves several methods. These include medications, device therapies, and lifestyle changes. We will explain the current treatments and why they are used.
Medications like beta-blockers and anti-arrhythmic drugs help control heart rate and rhythm. Sometimes, devices like pacemakers or ICDs are needed.
We work with patients to create a treatment plan that meets their needs. Our goal is to improve their quality of life.
Symptom 5: Dizziness, Lightheadedness, and Fainting
As cardiac amyloidosis gets worse, people might feel dizzy, lightheaded, or faint. These signs show that blood pressure might not be working right. It’s important to manage these symptoms well.
Blood Pressure Abnormalities in Cardiac Amyloidosis
Blood pressure problems are common in cardiac amyloidosis. They can cause dizziness and fainting. This happens because the heart can’t control blood pressure well due to amyloid deposits.
People with cardiac amyloidosis might have low or high blood pressure. This depends on how much amyloid is in the heart and how it affects the body.
Orthostatic Hypotension and Syncope
Orthostatic hypotension is a big worry for those with cardiac amyloidosis. It leads to syncope, or fainting. This happens when blood pressure drops too much when standing up, not enough blood reaches the brain.
|
Symptoms |
Causes |
Management Strategies |
|---|---|---|
|
Dizziness, lightheadedness |
Orthostatic hypotension, autonomic dysfunction |
Increase fluid intake, adjust medications, use compression stockings |
|
Fainting (syncope) |
Severe orthostatic hypotension, cardiac arrhythmias |
Fall prevention measures, medication adjustment, pacemaker implantation in some cases |
Safety Considerations and Prevention
To deal with dizziness, lightheadedness, and fainting, there are steps to take. Stand up slowly, drink plenty of water, and wear compression stockings. These can help prevent problems.
It’s key for patients with cardiac amyloidosis to work with their doctors. They should have a plan to check blood pressure and adjust medicines as needed.
Diagnostic Approaches and Treatment Options for Cardiac Amyloidosis
Diagnosing cardiac amyloidosis involves several steps. We use imaging, biomarkers, and tissue biopsies. This detailed approach helps us find the right treatment.
Non-Invasive Diagnostic Tests
Non-invasive tests are key in diagnosing cardiac amyloidosis. These include:
- Echocardiography: Shows heart structure and function.
- Cardiac MRI: Gives detailed heart images, spotting amyloid deposits.
- Electrocardiography (ECG): Reveals abnormal heart rhythms.
- Biomarkers: Blood tests for cardiac troponin and NT-proBNP, which can be high in cardiac amyloidosis.
Tissue Diagnosis Methods
Confirming amyloid deposits in the heart is vital. The main method is endomyocardial biopsy. This takes a heart tissue sample for examination. Other tissues like fat or bone marrow may also be biopsied to support the diagnosis.
Current Treatment Approaches
Treatment for cardiac amyloidosis depends on the type and stage. Current methods include:
|
Treatment Type |
Description |
Application |
|---|---|---|
|
Transthyretin Stabilizers |
Medications that stabilize transthyretin protein |
Used for hereditary transthyretin amyloidosis |
|
Chemotherapy |
Treatments that target plasma cell dyscrasias |
Applied in light chain amyloidosis |
|
Supportive Care |
Management of symptoms and complications |
Used across various types of cardiac amyloidosis |
Emerging Therapies and Clinical Trials
New treatments for cardiac amyloidosis are being researched. These include transthyretin stabilizers, gene therapies, and immunotherapies. Joining clinical trials can give patients early access to these treatments.
Our understanding of cardiac amyloidosis is growing. This means new diagnostic and treatment options are emerging. It’s important for healthcare providers and patients to stay updated on these advancements.
Conclusion: Living with Cardiac Amyloidosis
Cardiac amyloidosis is a serious condition where amyloid proteins build up in the heart. This leads to restrictive cardiomyopathy and can be life-threatening. It’s important to know the symptoms early to manage it well.
Managing cardiac amyloidosis means making lifestyle changes and getting ongoing medical care. It’s key to recognize symptoms like shortness of breath, fatigue, and swelling. This helps get medical help quickly.
Early detection and proper management can greatly improve life for those with cardiac amyloidosis. Patients can work with their doctors to create a treatment plan. This plan should include the latest in cardiac amyloidosis treatment.
We are dedicated to helping those with cardiac amyloidosis. By understanding the condition and its symptoms, we can improve outcomes. Together, we can make life better for those with amyloid heart disease.
FAQ
What is cardiac amyloidosis?
Cardiac amyloidosis is a condition where abnormal proteins, called amyloid, build up in the heart. This makes the heart stiff and can be very dangerous.
What are the main types of cardiac amyloidosis?
There are three main types. These are light chain (AL) amyloidosis, transthyretin (ATTR) amyloidosis, and hereditary transthyretin amyloidosis (ATTRm).
What are the symptoms of cardiac amyloidosis?
Symptoms include shortness of breath and feeling very tired. You might also have swelling in your legs, an irregular heartbeat, and feel dizzy or faint.
How is cardiac amyloidosis diagnosed?
Doctors use tests like echocardiography and cardiac MRI to diagnose it. They also do biopsies to confirm the diagnosis.
What are the treatment options for cardiac amyloidosis?
Treatment includes managing symptoms and slowing the disease’s progress. In some cases, there are targeted therapies to help.
Can cardiac amyloidosis be cured?
There is no cure yet. But early detection and treatment can greatly improve a patient’s life.
What is the role of genetic predisposition in cardiac amyloidosis?
Genetics play a big role, mainly in hereditary transthyretin amyloidosis (ATTRm). Certain mutations can cause the condition.
How does age relate to the risk of developing cardiac amyloidosis?
The risk goes up with age. Most cases happen in people over 60.
What are the possible complications of untreated cardiac amyloidosis?
Untreated, it can lead to heart failure and arrhythmias. These can be very serious and even life-threatening.
Are there any emerging therapies for cardiac amyloidosis?
Yes, new treatments and clinical trials are being developed. They aim to slow or stop the disease’s progress.
How can patients manage symptoms of cardiac amyloidosis?
Patients can manage symptoms by making lifestyle changes. This includes conserving energy, managing swelling, and following treatment plans.
What is the importance of early detection in cardiac amyloidosis?
Early detection is key. It allows for timely treatment and management, improving outcomes and quality of life.
References
National Center for Biotechnology Information. Cardiac Amyloidosis: Key Symptoms and Diagnostic Considerations. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7095437/










