Behavioral variant frontotemporal dementia (bvFTD) is a serious brain disease. It changes how people behave and think. It usually hits people between 45 and 65, often mistaken for a mental illness. Understand the BVFTD stages and the 5 extreme behavior changes that can occur. Crucial information for caregivers of those with behavioral variant FTD.
The bvFTD symptoms can be very extreme. They affect how people act, feel empathy, and make decisions. As the disease gets worse, these changes grow harder to handle for everyone involved.
It’s key to know about the big changes in frontotemporal dementia behavioral variant. We’ll dive into these changes. This will help us understand the disease better and support those affected and their families.
Key Takeaways
- bvFTD is a progressive neurodegenerative disorder affecting behavior and personality.
- The condition typically affects individuals between 45 and 65 years old.
- bvFTD symptoms include significant changes in social conduct and empathy.
- Early diagnosis is challenging due to similarities with psychiatric conditions.
- Understanding bvFTD symptoms is key for effective management and support.
Understanding Behavioral Variant Frontotemporal Dementia

bvFTD is a leading cause of dementia in people under 65. It causes unique changes in behavior and thinking. This type of dementia affects personality, behavior, and social actions.
Definition and Neurological Basis
bvFTD damages the brain’s frontal and temporal lobes. These areas are key for personality, behavior, and language. This damage leads to a decline in social behavior and emotional control.
The symptoms of bvFTD mainly come from the frontal lobe’s atrophy. This lobe handles decision-making and impulse control. The temporal lobe, which is also affected, is important for language and emotions.
Prevalence and Demographics in the United States
About 50,000 to 60,000 people in the U.S. have bvFTD. It’s a big cause of dementia in younger people. But, it’s often misdiagnosed or confused with other conditions.
bvFTD usually starts between 45 and 65 years old. It can also start in younger or older people. Men and women are affected equally, but some studies show a slight increase in men.
Distinguishing bvFTD from Alzheimer’s Disease
It’s important to tell bvFTD apart from Alzheimer’s disease. Both cause dementia, but they show different symptoms. Alzheimer’s mainly affects memory, while bvFTD changes behavior and personality.
bvFTD patients often lose empathy and show compulsive behaviors. These are not early signs of Alzheimer’s. To diagnose bvFTD, doctors need to do a thorough check-up, including brain scans and tests.
The Clinical Progression of BVFTD Stages

It’s important to understand how bvFTD progresses. This knowledge helps patients and caregivers manage the condition better. The disease goes through different stages, with symptoms getting worse over time. Early detection and action are key to improving life for those affected.
Prodromal and Early Stage Manifestations
In the early stages, small changes in behavior and personality may start. These can include mild disinhibition, apathy, or changes in eating habits. As the disease moves to the early stage, these symptoms get stronger.
Patients may show inappropriate social behavior, lack of empathy, or compulsive actions. Families often notice big changes in their loved ones during this time.
Middle Stage Progression
In the middle stage, symptoms get worse, and patients show more behavioral changes. This can include more disinhibition, compulsive behaviors, and less social interaction. Caregivers need to create structured care plans to manage these symptoms well.
Advanced Stage Symptoms
In the advanced stage, patients need full-time care. Symptoms include severe apathy, loss of empathy, and cognitive decline. They may also have motor symptoms like walking or swallowing problems. At this point, the focus is on comfort and pain management.
Average Disease Timeline
The timeline for bvFTD varies a lot. On average, patients live 6-11 years after symptoms start. But it can be as short as 2 years or as long as over 20 years. Knowing the average timeline helps healthcare providers and families plan for the future.
Every patient’s journey with bvFTD is different. Understanding the progression helps us support those affected better. This way, we can improve their quality of life.
“The progression of bvFTD is a challenging journey for both patients and caregivers, requiring compassion, understanding, and complete care.”
Disinhibition: When Social Filters Disappear
Disinhibition in bvFTD patients means they lose their social filters. This affects both patients and their caregivers. Damage to the frontal lobe leads to a loss of social restraint. This shows in various problematic behaviors.
Inappropriate Comments and Social Behaviors
Disinhibition often leads to saying or doing things that are not okay. Patients might say something offensive or do something considered taboo. These actions can upset family and caregivers.
For example, a patient might make a rude comment or touch someone inappropriately. These behaviors can hurt the patient’s social life and relationships.
Impulsive Actions and Risky Decision-Making
Disinhibition also causes impulsive actions and risky decisions. Patients might spend money recklessly, make sudden travel plans, or take dangerous risks. These actions can be harmful to themselves and others.
It’s important for caregivers to find ways to manage these behaviors. This helps keep everyone safe.
How Disinhibition Evolves Across Disease Stages
Disinhibition changes as bvFTD progresses. In the early stages, patients might make occasional inappropriate comments.
As the disease gets worse, these behaviors become more common and severe. Knowing how disinhibition changes helps caregivers plan better.
|
Disease Stage |
Disinhibition Manifestations |
Management Strategies |
|---|---|---|
|
Early Stage |
Mild inappropriate comments, occasional impulsive decisions |
Monitoring, gentle redirection |
|
Middle Stage |
More frequent inappropriate behaviors, increased impulsivity |
Structured environment, caregiver support |
|
Advanced Stage |
Severe disinhibition, significant impulsivity, possible safety risks |
Close supervision, safety measures, professional caregiver help |
Management Strategies for Caregivers
Caregivers are key in managing bvFTD disinhibition. Creating a structured environment and setting clear rules helps. This can reduce some of the tough behaviors.
Seeking help from professional caregivers and support groups is also helpful. It helps caregivers deal with the stress and challenges of caring for someone with bvFTD.
Apathy and Emotional Blunting: The Silent Symptom
In bvFTD, apathy and emotional blunting often hide behind more obvious changes. Apathy affects up to 84% of patients, greatly impacting their life quality.
Recognizing Apathy in Early bvFTD
Spotting apathy early is key for quick help. Apathy in bvFTD means less motivation and starting things less often. It’s different from depression, which includes sadness.
Diminished Motivation and Initiative
People with bvFTD show less drive and start things less. They might lose interest in things they used to like. Caregivers see them seeming not to care or be disconnected.
Progression of Apathy Through Disease Stages
Apathy gets worse as bvFTD gets worse. At first, it’s small, but later, it’s a big problem. It affects patient care and the burden on caregivers.
Approaches to Engagement and Stimulation
Helping patients with bvFTD needs many ways. Try structured activities, social time, and familiar routines to spark interest. Caregivers are key in changing these plans as the disease grows.
Understanding apathy in bvFTD helps us make better care plans. This improves patients’ lives and helps their caregivers too.
Loss of Empathy and Emotional Disconnection
One of the toughest parts of bvFTD is losing empathy. This affects how patients connect with others. It’s key to know why this happens and how it impacts both patients and their caregivers.
Reduced Response to Others’ Needs and Feelings
People with bvFTD often show less concern for others’ feelings. This isn’t because they don’t care. It’s because their brains are damaged by bvFTD.
Caregivers see their loved ones not responding to emotional needs. For example, a patient might not comfort a family member when they’re upset. Or they might not react right to big events.
Changes in Emotional Recognition Abilities
bvFTD also makes it hard for patients to recognize and interpret emotions in others. This can cause misunderstandings and wrong responses in social situations.
- Difficulty understanding facial expressions
- Challenges in interpreting tone of voice
- Reduced ability to empathize with others’ feelings
Stage-Specific Manifestations of Empathy Loss
The way bvFTD affects empathy changes over time. In the early stages, patients might show some empathy, but less than before. As the disease gets worse, they find it harder to empathize.
|
Disease Stage |
Empathy Loss Manifestations |
|---|---|
|
Early Stage |
Mild reduction in empathetic responses |
|
Middle Stage |
Noticeable decline in emotional understanding |
|
Advanced Stage |
Significant loss of empathetic abilities |
Preserving Emotional Connections with Patients
Even with bvFTD’s challenges, caregivers can keep emotional bonds strong. They can do this by:
- Maintaining a consistent routine
- Using non-verbal communication, such as touch
- Engaging patients in activities they enjoy
Understanding how bvFTD changes emotional processing helps caregivers. They can then find ways to support their loved ones and keep their relationships meaningful.
Compulsive Behaviors and Altered Eating Patterns
Patients with bvFTD face challenges with compulsive behaviors and eating changes. It’s key to understand how the disease affects them. This knowledge helps both patients and caregivers.
Repetitive Movements and Ritualistic Actions
People with bvFTD may do the same thing over and over. These actions are often not under their control. They can be upsetting for the person and their family.
Repetitive movements might include hand clapping or pacing. These actions can take up a lot of a person’s day.
As the disease gets worse, these behaviors can change. It’s important for caregivers to keep up with these changes. This helps in finding better ways to care for the patient.
Hyperorality and Dietary Changes
People with bvFTD might want to eat or drink a lot. They don’t always choose the right foods. This can lead to weight changes and health problems.
They might also want sweet or starchy foods more. This makes it harder to manage their diet. Caregivers need to watch what they eat to avoid problems.
Evolution of Compulsive Symptoms Across Stages
Compulsive behaviors and eating changes in bvFTD get worse over time. At first, they might not be very noticeable. But as the disease gets worse, they can become harder to handle.
- Early stages: Symptoms may be mild and intermittent.
- Middle stages: Behaviors can become more frequent and disruptive.
- Advanced stages: Symptoms often require significant caregiver intervention.
Safety Considerations and Interventions
Dealing with compulsive behaviors and eating changes needs a careful plan. Caregivers must think about safety considerations. This includes making sure the patient doesn’t eat too much or get into dangerous things.
Interventions might include:
- Structured routines to reduce the occurrence of compulsive behaviors.
- Dietary management strategies to prevent overeating or consumption of inappropriate items.
- Monitoring and adapting to the patient’s changing needs over time.
By understanding and tackling these symptoms, caregivers can make life better for patients and themselves.
Personality Transformation: The Core of BVFTD
bvFTD brings about extreme changes in behavior, leading to deep personality shifts. These changes are not just on the surface. They are a real transformation in how a person acts and feels.
Fundamental Character Alterations
The changes in bvFTD can make a person seem like a completely different person. They may start acting in ways that are out of character and could be harmful. This can include becoming more aggressive, apathetic, or developing compulsive behaviors.
For example, someone who was always calm might start getting angry easily. It’s important for families to understand these changes to offer the right support.
Loss of Self-Awareness and Insight
One of the toughest parts of bvFTD is when patients lose awareness of their own changes. They might not see how their actions affect others. This makes it hard for caregivers to help, as patients may not accept help or see the problem.
Caregivers often feel frustrated because the person they knew is gone. They can’t meet their needs in the same way anymore.
Stage-Related Personality Changes
As bvFTD progresses, personality changes grow more obvious. In the early stages, small changes might be noticed, like a slight change in social behavior or less empathy. As the disease gets worse, these changes get bigger.
|
Disease Stage |
Personality Changes |
|---|---|
|
Early Stage |
Subtle changes in social behavior, decreased empathy |
|
Middle Stage |
More pronounced behavioral changes, increased apathy or aggression |
|
Advanced Stage |
Significant loss of self-awareness, severe behavioral disturbances |
Helping Families Cope with “Different Person” Syndrome
Families dealing with bvFTD face a big challenge. Support groups and counseling are key in helping them cope. Learning about the disease and its effects can help families understand and be patient.
Keeping a routine and reducing stress can also help manage symptoms. This can make life easier for both the person with bvFTD and their family.
Diagnosis, Treatment, and Management Approaches
Getting a correct diagnosis and managing bvFTD well is key to better patient outcomes. It’s hard to diagnose bvFTD because it looks like other brain diseases. A detailed approach is needed.
Current Diagnostic Criteria and Challenges
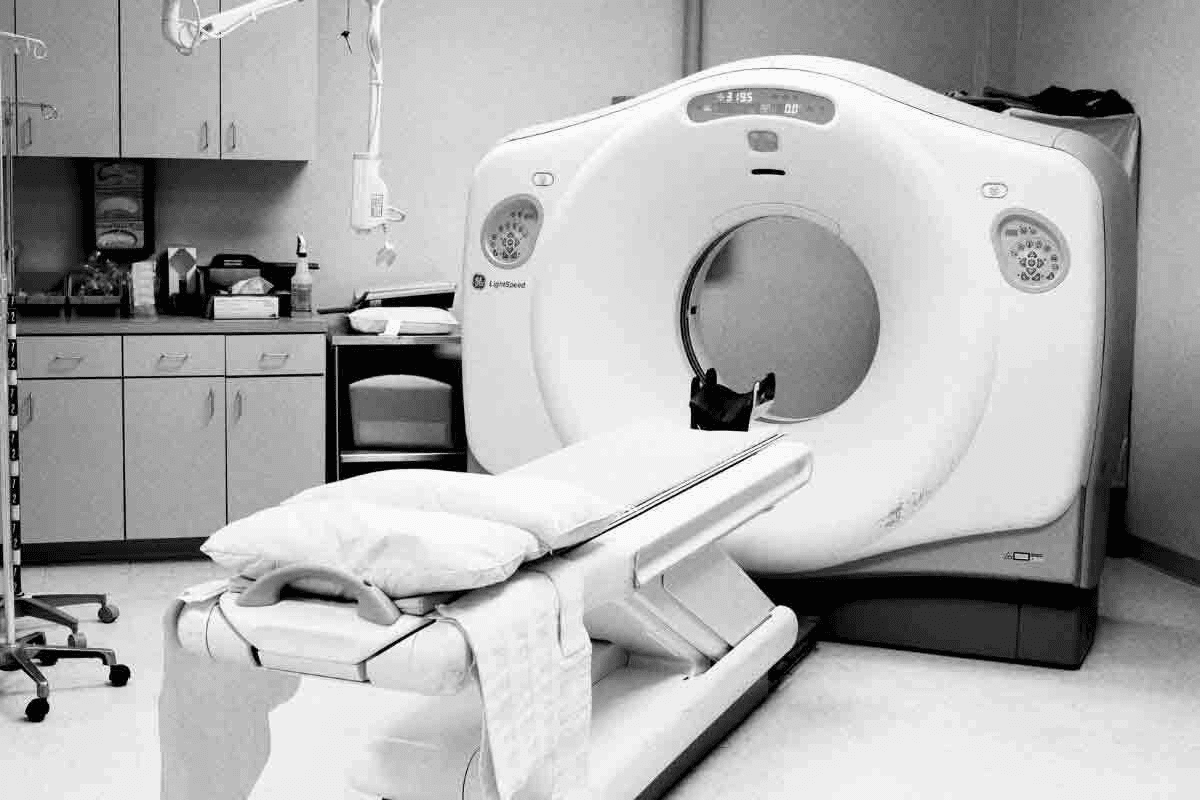
To diagnose bvFTD, doctors use clinical checks, brain tests, and imaging. The criteria include big changes in behavior or personality, like acting out, being very apathetic, or having compulsive actions.
Even with progress, diagnosing bvFTD is tough because it can look like other conditions. Early and accurate diagnosis is vital for the right care and support.
|
Diagnostic Criteria |
Clinical Features |
|---|---|
|
Behavioral Changes |
Disinhibition, apathy, compulsive behaviors |
|
Neuropsychological Testing |
Executive function deficits, memory impairment |
|
Imaging Studies |
Frontal and temporal lobe atrophy |
Pharmacological Interventions for Behavioral Symptoms
Medicines are used to handle bvFTD’s behavioral issues, like agitation, aggression, and sadness. SSRIs are often given for these symptoms.
Other drugs, like antipsychotics and mood stabilizers, might be used for severe issues. But, their side effects must be carefully thought about.
Non-Pharmacological Management Strategies
Non-medical ways to manage bvFTD are very important. These include behavioral plans, support for caregivers, and making the environment less stressful.
Caregivers should set routines, talk clearly, and make a safe, supportive space. Education and support for caregivers are key to handling bvFTD’s challenges.
Emerging Research and Clinical Trials
Research on bvFTD is ongoing, with many clinical trials looking into new treatments. New therapies aim to tackle the disease’s root causes, possibly slowing it down.
Joining clinical trials offers new treatments and helps us understand bvFTD better. This improves care for those affected by it.
Conclusion: Supporting Patients and Caregivers Through the BVFTD Journey
Supporting patients and caregivers with bvFTD is key to bettering their lives. It’s not just about treating symptoms. It’s also about giving emotional and practical help.
Knowing about bvFTD helps us support better. We can improve care for both patients and caregivers. This means spotting behavioral changes and finding ways to handle them.
Helping those with bvFTD and their caregivers needs a full plan. We must tackle the many challenges they face. This way, we can help them get the best care possible.
FAQ
What is Behavioral Variant Frontotemporal Dementia (bvFTD)?
Behavioral Variant Frontotemporal Dementia (bvFTD) is a brain disorder. It changes how people behave and think. It usually starts in people between 45 and 65 years old.
How does bvFTD differ from Alzheimer’s disease?
bvFTD affects the brain’s frontal and temporal lobes. This leads to big changes in behavior. Alzheimer’s mainly hurts memory.
What are the stages of bvFTD?
bvFTD has four stages: prodromal, early, middle, and advanced. Each stage gets worse, with more behavior and thinking problems.
What is disinhibition in bvFTD?
Disinhibition in bvFTD means saying or doing things that are not right. It includes making bad choices and acting impulsively. These actions get worse as the disease gets worse.
How does apathy manifest in bvFTD?
Apathy in bvFTD means not wanting to do things. It’s hard to get someone with bvFTD to start or keep doing things. Knowing how it gets worse helps find ways to keep them engaged.
What is the impact of bvFTD on emotional recognition and empathy?
bvFTD can make it hard to understand and feel emotions. It’s important to find ways to keep emotional connections strong.
What are compulsive behaviors in bvFTD?
Compulsive behaviors in bvFTD include doing the same thing over and over. It also includes acting in certain ways and being overly focused on certain things. These behaviors get worse and need careful handling.
How does bvFTD affect personality?
bvFTD can change a person’s personality a lot. It can make them lose touch with who they are. It’s important to support families going through these changes.
What are the current diagnostic criteria for bvFTD?
To diagnose bvFTD, doctors look at how someone acts and thinks. It’s hard to tell it apart from other brain diseases.
What are the treatment and management approaches for bvFTD?
Treating bvFTD includes medicines for behavior and other ways to manage symptoms. There’s also new research and trials happening.
What is Pick’s disease, and how is it related to bvFTD?
Pick’s disease is a type of frontotemporal dementia. It has its own signs and is often seen as part of bvFTD.
How prevalent is bvFTD in the United States?
In the United States, bvFTD affects about 50,000 to 60,000 people. It has a big impact on patients, their families, and caregivers.
References
National Center for Biotechnology Information. Frontotemporal Dementia: Life Expectancy After Diagnosis. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3953732/