Frontotemporal dementia (FTD) is a brain disease that changes how people act, think, and move. It affects the frontal and temporal lobes. Getting diagnosed with FTD is very hard, as it often happens when people are at their most active years. Understand the frontal lobe dementia lifespan with essential facts for caregivers. Learn the prognosis and how to provide the best possible support.
Knowing what to expect is key for good care planning. Life expectancy with FTD varies a lot based on the disease type and personal factors. Even though most people with FTD live 7 to 13 years after being diagnosed, outcomes can vary a lot.
Key Takeaways
- FTD is a progressive brain disease affecting behavior, personality, language, and movement.
- Life expectancy with FTD varies depending on disease subtype and individual factors.
- Most people with FTD live 7 to 13 years after diagnosis.
- Understanding FTD prognosis is key for care planning.
- FTD usually affects people when they are at their most active years.
Understanding Frontotemporal Dementia (FTD)
Frontotemporal dementia is a group of rare brain disorders. It’s a major cause of early dementia. It damages the frontal and temporal lobes, causing cognitive, behavioral, and motor symptoms.
What Is Frontotemporal Dementia?
FTD is a group of disorders that damage the frontal and temporal lobes. This damage causes brain shrinkage. It affects behavior, language, and motor skills.
FTD is often mistaken for Alzheimer’s disease. This is because their symptoms can be similar.
How FTD Differs from Other Dementias
FTD is different from other dementias like Alzheimer’s. It starts early and affects personality, behavior, and language first. People with FTD usually start showing symptoms between 40 and 65 years old.
FTD has several subtypes. These are based on the main symptoms:
- Behavioral variant FTD (bvFTD), characterized by changes in personality and behavior.
- Primary Progressive Aphasia (PPA), affecting language skills.
- FTD with motor neuron disease, which includes symptoms of motor neuron disease, such as muscle weakness.
Who Is Typically Affected by FTD?
FTD is rare, affecting 15 to 22 per 100,000 people under 65. It’s a common cause of early dementia. It often strikes people in their 50s, when they are working and raising families.
|
Characteristics |
FTD |
Alzheimer’s Disease |
|---|---|---|
|
Typical Age of Onset |
40-65 years |
65+ years |
|
Primary Symptoms |
Changes in personality, behavior, and language |
Memory loss |
|
Progression |
Varies by subtype |
Gradual decline |
Knowing about FTD is key for diagnosis and care. Recognizing its unique characteristics helps healthcare providers offer better support. This is for both the person with FTD and their family.
Types of Frontotemporal Dementia and Their Impact on Survival

Knowing the different types of FTD is key to understanding patient outcomes. Each subtype of frontotemporal dementia has its own set of symptoms and survival rates.
Behavioral Variant FTD (bvFTD)
Behavioral variant FTD is the most common type. It changes a person’s personality, behavior, and social skills. People with bvFTD might act impulsively, feel less motivated, or have compulsive behaviors. Their life expectancy after diagnosis can range from 6 to 14 years, depending on several factors.
Primary Progressive Aphasia (PPA)
Primary Progressive Aphasia mainly affects a person’s ability to use language. There are different types of PPA, like semantic and nonfluent variants. How fast PPA progresses can vary a lot, with some people experiencing a slower decline in language skills.
Semantic Dementia
Semantic dementia is a type of FTD that makes it hard to understand words and recognize objects and faces. Despite losing semantic knowledge, people with semantic dementia can often do daily tasks well.
FTD with Motor Neuron Disease (FTD-MND/ALS)
FTD-MND/ALS is a fast-moving type that combines FTD symptoms with ALS motor symptoms. This combination makes survival much shorter, with a median of about 2-3 years after diagnosis.
The survival times for all FTD types range from 7 to 13 years in clinical settings. This shows how important it is to know the specific type of FTD for better planning and care.
|
FTD Subtype |
Primary Characteristics |
Median Survival from Diagnosis |
|---|---|---|
|
Behavioral Variant FTD (bvFTD) |
Changes in personality, behavior, and social conduct |
6-14 years |
|
Primary Progressive Aphasia (PPA) |
Progressive decline in language abilities |
Varies significantly |
|
Semantic Dementia |
Loss of semantic knowledge, difficulty understanding word meanings |
Variable, often slower decline |
|
FTD with Motor Neuron Disease (FTD-MND/ALS) |
Cognitive and behavioral changes with motor symptoms |
2-3 years |
It’s vital to consider these differences when talking to patients and their families about what to expect and how to plan for their care.
Average Frontal Lobe Dementia Lifespan: What Research Shows
The lifespan of those with frontal lobe dementia varies a lot. Research on frontotemporal dementia (FTD) has given us important insights. It helps patients, caregivers, and doctors know what to expect.
Overall Survival Statistics
Studies show that FTD patients’ survival times can vary a lot. On average, they live 6 to 11 years after symptoms start. But, this time can be shorter or longer based on the FTD subtype and other health issues.
Survival rates depend on the FTD subtype. Knowing these differences is key for managing expectations and planning care.
Comparing Survival Rates Across FTD Subtypes
Each FTD subtype has its own survival profile. For example, FTD-MND/ALS has a shorter survival time than semantic dementia. Here’s what research says:
- FTD-MND/ALS: usually 2-3 years after symptoms start
- Behavioral variant FTD (bvFTD): about 6-8 years
- Semantic dementia: often 8-12 years or more
These differences show why accurate diagnosis and subtype identification are so important for predicting prognosis.
How FTD Survival Compares to Other Dementias
FTD progresses faster than other dementias, like Alzheimer’s. Alzheimer’s can last 8-15 years or more from diagnosis to death. But, FTD’s path is usually shorter, making timely and proper care even more critical.
Knowing these differences is essential for providing the best support for patients and their families. It helps tailor care to the specific needs and disease progression rate.
Factors That Influence Life Expectancy in FTD
Many things affect how long someone with Frontotemporal Dementia (FTD) lives. Knowing these can help patients, caregivers, and doctors manage the disease better.
Age at Diagnosis
When someone is diagnosed with FTD matters a lot. People diagnosed younger usually live longer than those diagnosed older. This is because younger people are often healthier and can fight the disease better.
Genetic Factors and Family History
Genetics are a big deal in FTD. If your family has FTD, you might get it too. Genetic tests can find genes that cause FTD. Knowing this can help plan care and treatments.
Presence of Comorbidities
Having other health problems can really affect FTD patients. Things like heart disease, diabetes, or breathing issues can make the disease worse. It’s important to manage these to improve life and maybe live longer.
Access to Specialized Care
Getting the right care is key for FTD patients. Doctors who know about dementia can make treatment plans that help. Teams of doctors can meet the complex needs of FTD patients better.
By understanding and tackling these factors, we can manage FTD better. This improves the lives of those with the disease.
The Impact of Early Detection on FTD Prognosis
Getting a Frontotemporal Dementia (FTD) diagnosis is tough. But catching it early can make a big difference. We know how hard it is to spot FTD and why acting fast is key.
Challenges in Diagnosing FTD
FTD is hard to diagnose because its symptoms can look like other diseases. Getting it right needs a detailed check-up, including tests and scans.
FTD symptoms can be confused with Alzheimer’s or other mental health issues. Special tools and experts are needed to tell FTD apart.
How Diagnostic Timing Affects Outcomes
When FTD is caught early, it makes a big difference. Quick action means better care and support for patients and their families.
Waiting too long to get a diagnosis can lead to missing out on important care. Acting fast also means more chances to try new treatments.
Biomarkers and Predictive Testing
Scientists are working on biomarkers and tests to spot FTD sooner. Biomarkers could find FTD before symptoms show, helping to start treatment early.
Tests for genetic FTD can find the cause. Genetic counseling is important for those getting tested.
|
Diagnostic Approach |
Description |
Benefits |
|---|---|---|
|
Clinical Assessments |
Comprehensive evaluation of patient symptoms and medical history |
Helps rule out other conditions |
|
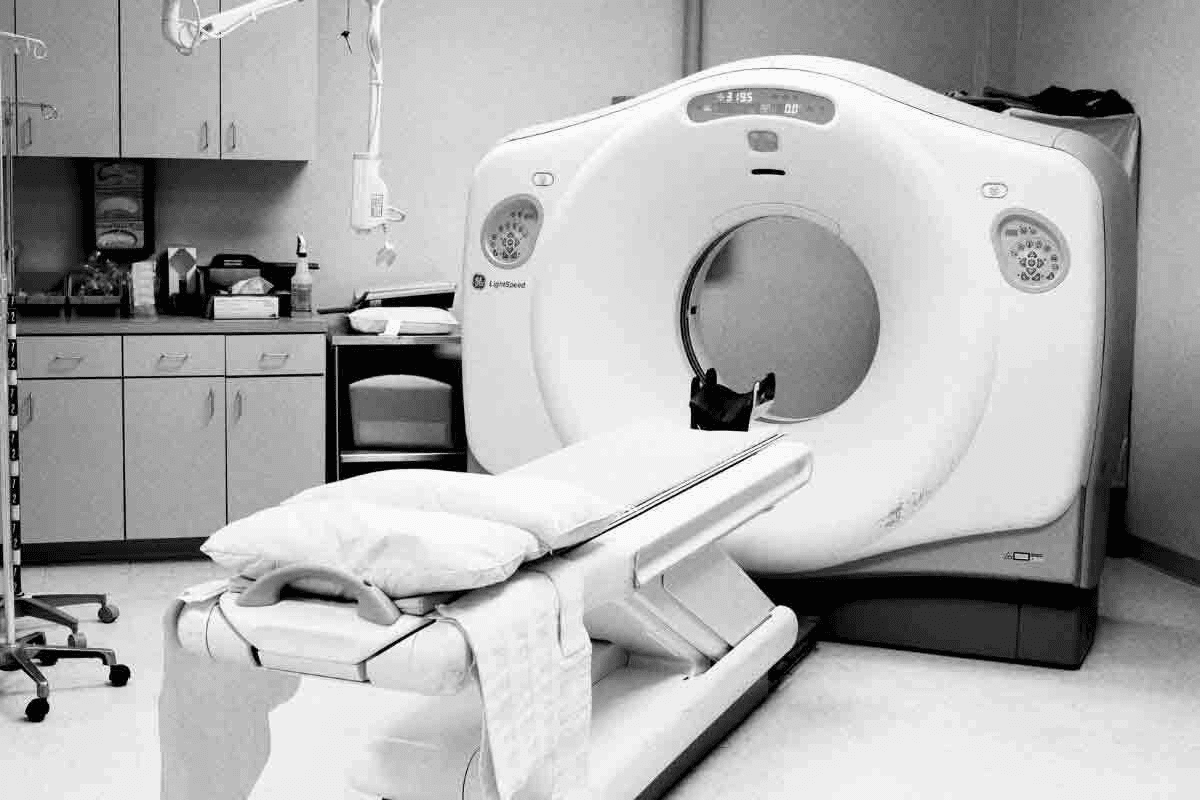
Imaging Studies |
Use of MRI or CT scans to assess brain changes |
Supports diagnosis by identifying characteristic FTD patterns |
|
Genetic Testing |
Identification of genetic mutations associated with FTD |
Facilitates diagnosis and predictive testing for familial cases |
Common Causes of Death in Frontotemporal Dementia
It’s important to know the common causes of death in frontotemporal dementia (FTD). This knowledge helps in managing the disease and improving care for patients. FTD patients face risks like respiratory failure, heart problems, and infections.
Respiratory Complications
Respiratory issues are a big risk for FTD patients. As the disease gets worse, swallowing problems can lead to pneumonia. We need to watch for signs of breathing trouble and take steps to prevent it.
Cardiovascular Issues
Heart problems are another major risk for FTD patients. The disease can mess with heart rate and blood pressure. We should watch for heart attacks and strokes and manage heart risks.
Nutritional Decline and Cachexia
Nutritional problems and cachexia are common in advanced FTD. These issues come from swallowing problems, less appetite, and more energy use. It’s key to keep patients well-nourished to avoid more problems. Sometimes, we need to use gastrostomy tubes to help with feeding.
Infections and Other Complications
Infections like pneumonia and urinary tract infections are common in FTD patients. The disease can also cause falls and fractures, which can shorten life expectancy. We must act fast to prevent and manage these issues to improve patient outcomes.
|
Cause of Death |
Description |
Management Strategies |
|---|---|---|
|
Respiratory Complications |
Aspiration pneumonia, respiratory failure |
Monitoring for dysphagia, aspiration precautions |
|
Cardiovascular Issues |
Autonomic dysfunction, heart attacks, strokes |
Managing cardiovascular risk factors |
|
Nutritional Decline and Cachexia |
Dysphagia, decreased appetite, cachexia |
Alternative feeding methods, nutritional support |
|
Infections and Other Complications |
Pneumonia, urinary tract infections, falls, fractures |
Proactive infection prevention, fall prevention strategies |
Understanding the common causes of death in FTD helps us manage the disease better. Early detection and action are key to reducing risks and improving patient care.
The Progression of FTD: Stages and Timeline
Knowing the stages of FTD is key for those affected and their caregivers. Frontotemporal dementia (FTD) changes behavior, language, and motor skills over time. It’s a complex neurodegenerative disorder.
FTD’s progression is different for everyone. It’s hard to guess exactly how long it will last. But, it goes through several stages, from the first signs to the most severe.
Early Stage Symptoms and Duration
In the early stages, symptoms are mild. You might notice small changes in behavior, language issues, or slight motor problems. How long this stage lasts can vary a lot, from months to years.
Getting an early diagnosis is very important. It helps start support and planning early. Patients and caregivers can get help with managing symptoms and planning for the future.
Middle Stage Progression
As FTD moves to the middle stage, symptoms get worse. You might see more obvious changes in behavior, like apathy or acting out. Language problems can make talking hard, and motor issues like weakness or coordination problems may start.
Supportive care is key in this stage. It’s about managing symptoms, keeping the patient comfortable, and ensuring their safety. Caregivers might need more help and resources to handle the care needs.
Advanced Stage and End-of-Life Care
In the advanced stage, patients need constant care because of big cognitive and motor problems. At this point, end-of-life care is all about comfort, dignity, and support for patients and their families.
Palliative care teams are very important here. They help with pain, nutrition, and emotional support.
Individual Variations in Disease Progression
How fast FTD progresses and what symptoms show up can differ a lot. Age at diagnosis, genetics, and other health issues can affect how the disease goes.
It’s important to understand these differences for personalized care and support. We’ll show how FTD can progress differently in the table below:
|
Stage |
Typical Symptoms |
Duration |
|---|---|---|
|
Early |
Mild behavioral changes, language difficulties |
Months to years |
|
Middle |
Pronounced behavioral changes, significant language impairment |
Years |
|
Advanced |
Significant cognitive and motor impairments |
Variable, often requiring full-time care |
In conclusion, FTD’s progression is complex and varies a lot. Knowing the stages and what affects them can help everyone involved deal with this tough disease.
How Treatments and Interventions May Affect FTD Prognosis
There’s no cure for Frontotemporal Dementia (FTD) yet. But, treatments can help manage symptoms and maybe extend life. How well these treatments work depends on the person and their FTD type.
Current Treatment Approaches
Today’s treatments aim to ease FTD symptoms. Medications like SSRIs help with behavior. We also use other meds for symptoms like agitation or depression.
For example, a patient with FTD and apathy might get a dopamine-boosting drug. Speech therapy is key for those with Primary Progressive Aphasia (PPA). It helps keep their communication skills going.
Symptom Management Strategies
Managing FTD symptoms needs a mix of strategies. We use behavioral interventions and change the environment to help patients and caregivers.
- Creating a daily routine to reduce confusion and agitation
- Implementing safety measures in the home to prevent accidents
- Using communication aids for patients with language difficulties
Emerging Research and Clinical Trials
Research on FTD is growing, with new areas to explore. Clinical trials are looking at treatments that could slow FTD down.
For instance, studies are looking at tau-targeting therapies for some FTD types. Advances in FTD genetics might lead to more tailored treatments soon.
Multidisciplinary Care Teams
A team of experts is key for FTD care. This team includes neurologists, psychiatrists, and more. They work together to meet FTD patients’ complex needs.
This teamwork can improve a patient’s life and maybe their prognosis. We think this team effort is vital for tackling FTD’s many challenges.
Conclusion
Understanding frontotemporal dementia (FTD) is key for patients, families, and doctors. The way FTD progresses and how long people live with it varies. This means each person needs care that fits their unique situation.
We’ve talked about the different types of FTD. These include behavioral variant FTD, primary progressive aphasia, and FTD with motor neuron disease. Each type affects survival in different ways. Things like age, genetics, and access to care also play big roles in how long someone with FTD might live.
Spotting FTD early is very important. It helps manage symptoms and can make life better for those with the disease. Knowing about FTD’s outlook helps doctors create better plans for treatment and care. This way, they can help improve the quality of life for those with FTD.
More research and better care for FTD are needed. Working together, we can make a big difference in the lives of those with FTD and their families.
FAQ
What is Frontotemporal Dementia (FTD) and how does it differ from other dementias?
Frontotemporal dementia is a rare brain disorder. It affects the frontal and temporal lobes. This leads to changes in personality, behavior, and language.
It’s different from Alzheimer’s disease because of its symptoms and age of onset. FTD usually starts at a younger age.
What are the different types of FTD and how do they impact survival?
There are several types of FTD, including Behavioral Variant FTD (bvFTD) and Primary Progressive Aphasia (PPA). Each type affects people differently.FTD-MND/ALS is the most severe. It combines FTD with motor neuron disease. This type progresses quickly.
What is the average lifespan of patients with frontal lobe dementia?
The lifespan of FTD patients varies. It depends on the type, age at diagnosis, and other health issues. On average, they live 6 to 12 years after symptoms start.But, it can be shorter or longer, up to over 20 years.
How does the age at diagnosis affect life expectancy in FTD?
The age at diagnosis is key. Younger patients usually live longer. Older patients have a shorter life expectancy.
What role do genetic factors play in FTD life expectancy?
Genetics are very important in FTD. Certain genes, like GRN and C9ORF72, affect when and how fast the disease progresses. Family history also matters, as it can increase the risk of getting FTD.
What are the common causes of death in FTD patients?
FTD patients often die from respiratory problems, heart issues, and infections. These issues come from the disease’s progression. It can cause swallowing problems, immobility, and weaken the immune system.
How does early detection impact FTD prognosis?
Finding FTD early can make a big difference. It allows for better management of symptoms and planning for the future. While there’s no cure, early diagnosis can improve life quality and slow the disease.
What are the current treatment approaches for FTD?
Today, treatments for FTD focus on managing symptoms and improving life quality. A team of healthcare professionals works together to create a care plan. This team includes neurologists and therapists.
Can FTD be prevented or slowed down?
There’s no sure way to prevent or slow FTD yet. But, research is ongoing. Lifestyle changes, like exercise and staying mentally active, might help some symptoms. More research is needed to know for sure.
What is the role of multidisciplinary care teams in managing FTD?
Multidisciplinary care teams are essential in managing FTD. They provide a coordinated approach to care. This team-based care improves outcomes, enhances life quality, and supports caregivers.
References
National Center for Biotechnology Information. Frontotemporal Dementia: Life Expectancy After Diagnosis. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3953732/