Many of us question if insomnia disorder is a real disease or just a sign of other health problems. Today, science has given us a clear answer. Insomnia disorder is seen as a unique sleep disorder with its own set of rules and serious health effects.
About one-third of adults deal with insomnia pathology, which is both complex and varied. It’s listed in the DSM-5 and International Classification of Sleep Disorders. Knowing if you or someone you care about has it is key to getting the right treatment.
Key Takeaways
- Insomnia disorder is a recognized sleep-wake disorder with distinct diagnostic criteria.
- It affects approximately one-third of adults worldwide.
- Understanding the symptoms and pathology is key for effective treatment.
- Evidence-based treatment can greatly improve your life quality.
- Classification in the DSM-5 and International Classification of Sleep Disorders helps in diagnosing.
Defining Insomnia Disorder: More Than Just Poor Sleep

Insomnia disorder is more than just bad sleep. It has its own set of rules for diagnosis. Knowing these rules helps us give the right treatment.
The Clinical Definition of Insomnia
The International Classification of Sleep Disorders defines insomnia disorder. It includes trouble starting to sleep, staying asleep, or feeling like you’re not sleeping well. This is key for doctors to treat insomnia right. Symptoms include trouble falling asleep, waking up a lot at night, and waking up too early.
“Insomnia disorder is a long-term problem with starting, staying, or feeling rested during sleep,” say sleep doctors. This shows how complex insomnia is, making it different from just having a bad night’s sleep.
Distinguishing Normal Sleep Variations from Disorder
Telling normal sleep issues from insomnia disorder is vital. Normal sleep can be off due to stress or where you sleep. But insomnia disorder lasts a long time and really affects your life.
Doctors look at how often and long sleep problems last, and how they affect daily life. Insomnia disorder is not just about how much you sleep. It’s also about the quality and how it affects you.
By knowing the definition and criteria of insomnia disorder, we can help those who have it. We can give them the care and support they need.
The Prevalence and Burden of Insomnia Disorder

It’s important to understand insomnia disorder’s impact. It’s a big public health issue that affects many people around the world.
Statistical Overview: Who Suffers from Insomnia?
About 6 to 10 percent of adults have insomnia bad enough to be diagnosed. Studies show that more women, older people, and those with health or mental issues get insomnia.
Insomnia affects different groups in different ways. For example:
- Women are more likely to get insomnia than men, possibly because of hormones and other factors.
- Older adults face a higher risk, possibly because of sleep changes and more health issues.
- People with long-term health or mental problems are more likely to get insomnia, showing how it’s linked to other health issues.
Economic and Social Burden
Insomnia disorder has big economic and social costs. It leads to:
- More visits to doctors, tests, and treatments, which costs a lot.
- Less work and more time off, which hurts the economy.
- Worse thinking skills and more accidents, which also costs society a lot.
Medical Expert, a sleep expert, said, “Insomnia is not just a sleep issue; it’s a health problem that affects many parts of life.” This shows we need better ways to handle insomnia.
In summary, insomnia’s impact is huge. We need more research, awareness, and ways to manage it to help people and society.
Clinical Presentation: Key Symptoms of Insomnia Disorder
It’s key to know the symptoms of insomnia disorder to diagnose and treat it well. This condition affects sleep quality and daily life. It impacts how well you function during the day and your overall happiness.
Difficulty Initiating Sleep
One main symptom is difficulty initiating sleep. People with insomnia find it hard to fall asleep, even when they’re tired. This can happen for many reasons, like being too stressed or having an irregular sleep schedule.
Difficulty Maintaining Sleep
Another symptom is difficulty maintaining sleep. People wake up during the night and can’t go back to sleep. This leads to broken sleep and doesn’t help you feel rested.
Early Morning Awakening
Early morning awakening is also common. People wake up too early and can’t fall back asleep. This shortens your sleep time and makes you feel more tired during the day.
Daytime Consequences and Functional Impairments
Insomnia’s effects aren’t just at night. They also affect you during the day. You might feel very sleepy, tired, and have mood swings. These feelings can make it hard to focus, remember things, and make decisions.
These problems can also make it hard to do daily tasks, work well, and interact with others. This can lower your quality of life.
Understanding both the nighttime and daytime effects of insomnia is vital. It helps in treating the condition fully.
The Evolution of Insomnia Classification in Medical Literature
Insomnia classification has a long history. It has changed as our understanding of sleep has grown. Now, we categorize insomnia in more complex and detailed ways.
Historical Perspectives on Insomnia
In the past, insomnia was seen as a symptom, not a condition on its own. Early systems grouped it with other sleep issues or psychiatric problems. It was thought to be caused by other medical or psychological issues.
As sleep medicine advanced, researchers saw insomnia as a unique condition. Studies showed how common and serious it was. This change marked a big step in how we classify insomnia.
The Shift from Primary/Secondary to Disorder-Based Classification
The old primary/secondary system had its flaws. It suggested that treating the main issue would fix insomnia. But, in reality, insomnia often stayed even after treating the cause.
The new disorder-based system sees insomnia as a condition that needs its own diagnosis and treatment. This change is seen in today’s medical guides, which list insomnia disorder as a separate condition.
Implications for Clinical Practice
The new way of classifying insomnia changes how doctors work. Recognizing insomnia as a distinct condition leads to better diagnosis and treatment. This approach means doctors look at the whole patient, not just the sleep issue.
This new classification also shapes treatment plans. There’s more focus on specific insomnia therapies, like Cognitive Behavioral Therapy for Insomnia (CBT-I). These methods have been proven to help patients sleep better and feel better overall.
Insomnia Disorder in Modern Diagnostic Systems
Today, we understand insomnia disorder in new ways. The rules for diagnosing it have changed. This shows how much we’ve learned about sleep problems and their effects on health.
DSM-5 Criteria and Classification
The DSM-5 gives clear rules for diagnosing insomnia. It says insomnia is hard to start or stay asleep, even when you have the chance. This makes you feel bad during the day or affects your work or life.
The DSM-5 criteria for insomnia include:
- Difficulty starting to sleep
- Struggling to stay asleep
- Waking up too early and can’t go back to sleep
- Symptoms must last at least 3 months
- Symptoms must happen at least 3 times a week
- Feeling really bad or having trouble with daily life
International Classification of Sleep Disorders (ICSD-3)
The ICSD-3 also has rules for diagnosing insomnia. It stresses the need for a detailed check-up. This includes looking at sleep diaries and checking for other sleep issues.
|
Diagnostic Criteria |
DSM-5 |
ICSD-3 |
|---|---|---|
|
Duration of Symptoms |
At least 3 months |
At least 3 months |
|
Frequency of Symptoms |
At least 3 times per week |
Not specified |
|
Daytime Consequences |
Significant distress or impairment |
Impairment in daytime functioning |
ICD-11 Approach to Insomnia
The ICD-11 changes how we classify insomnia. It has more detailed rules. It looks at how often and long symptoms last, and how they affect daily life.
Diagnostic Challenges and Considerations
Even with better rules, diagnosing insomnia is hard. Doctors need to look at the patient’s overall health and other sleep issues. A full check-up is key for a correct diagnosis and treatment plan.
Using sleep diaries, actigraphy, and other tools is important. Insomnia diagnosis is complex. It shows we need a deep understanding of the disorder and its effects on people.
The Pathophysiology of Insomnia Disorder
Insomnia disorder has a complex cause. It includes hyperarousal, changes in the brain, and genetic factors. Knowing these causes is key to finding good treatments.
Hyperarousal States and Sleep Disruption
Hyperarousal is a big part of insomnia. It means the body is too active, making it hard to sleep. Stress, anxiety, and lifestyle can cause it.
Hyperarousal makes it hard to start or stay asleep. It shows as a fast heart rate, high body temperature, and active brain. People with insomnia often have a very active sympathetic nervous system.
|
Characteristics |
Normal Sleep |
Insomnia Disorder |
|---|---|---|
|
Sympathetic Nervous System Activity |
Low |
High |
|
Cortical Activity |
Decreased |
Increased |
|
Body Temperature |
Lower |
Higher |
Neurobiological Mechanisms
Insomnia’s brain mechanisms are complex. They involve neurotransmitters and brain areas. The hypothalamic-pituitary-adrenal (HPA) axis and neurotransmitters like serotonin, norepinephrine, and GABA are key.
When these systems are off balance, it’s hard to relax and sleep. For example, too much excitatory neurotransmitters can make you feel too awake.
The Role of Neurotransmitters and Brain Activity
Neurotransmitters control when we sleep and wake. GABA helps us relax, while norepinephrine and serotonin make us more alert. The right balance is important for sleep.
In insomnia, this balance is often wrong. This leads to trouble sleeping and feeling too awake.
Genetic Factors in Insomnia Vulnerability
Genetics also play a part in insomnia. Some genes affect sleep and stress response. Knowing this can help find people at risk and create better treatments.
Psychological Mechanisms in Insomnia Disorder Development
Understanding the psychological reasons behind insomnia is key to treating it. Insomnia is more than just not sleeping well. It’s a complex issue influenced by many psychological factors.
Conditioned Arousal and Learned Sleep Difficulties
Conditioned arousal is a major factor in insomnia. This happens when the bed and bedroom become linked to stress and staying awake. Over time, people may find it hard to sleep because of this association.
Learned sleep difficulties also play a big role. People with insomnia often develop habits that make sleep harder. These habits include staying in bed too long, trying too hard to sleep, or doing stimulating activities before bed.
Cognitive Models of Insomnia
Negative thoughts and beliefs about sleep can keep insomnia going. People might worry about how poor sleep will affect them the next day. Or they might feel like they can’t control their sleep. These thoughts can make it even harder to fall asleep.
- Misattribution: Thinking sleep problems come from outside factors instead of looking at the real issues.
- Catastrophizing: Believing poor sleep will have terrible consequences.
- Rumination: Thinking too much about sleep issues, which can increase anxiety and worsen insomnia.
The Perpetuating Cycle of Sleep-Related Anxiety
The cycle of sleep-related anxiety is another important factor. Worrying about sleep makes it harder to fall asleep. This creates a cycle where fear of insomnia makes it worse.
To stop this cycle, we need to tackle the underlying psychological issues. Cognitive-behavioral therapy for insomnia (CBT-I) can help change sleep habits and reduce anxiety about sleep.
By understanding and tackling these psychological factors, we can create better treatments for insomnia. It’s a complex challenge, but it offers hope for those struggling with this condition.
Understanding Insomnia Disorder as a Comorbid Condition
It’s important to understand how insomnia disorder relates to other health issues. This is key for making the right diagnosis and treatment. Insomnia often goes hand in hand with other health problems, making it harder to diagnose and treat.
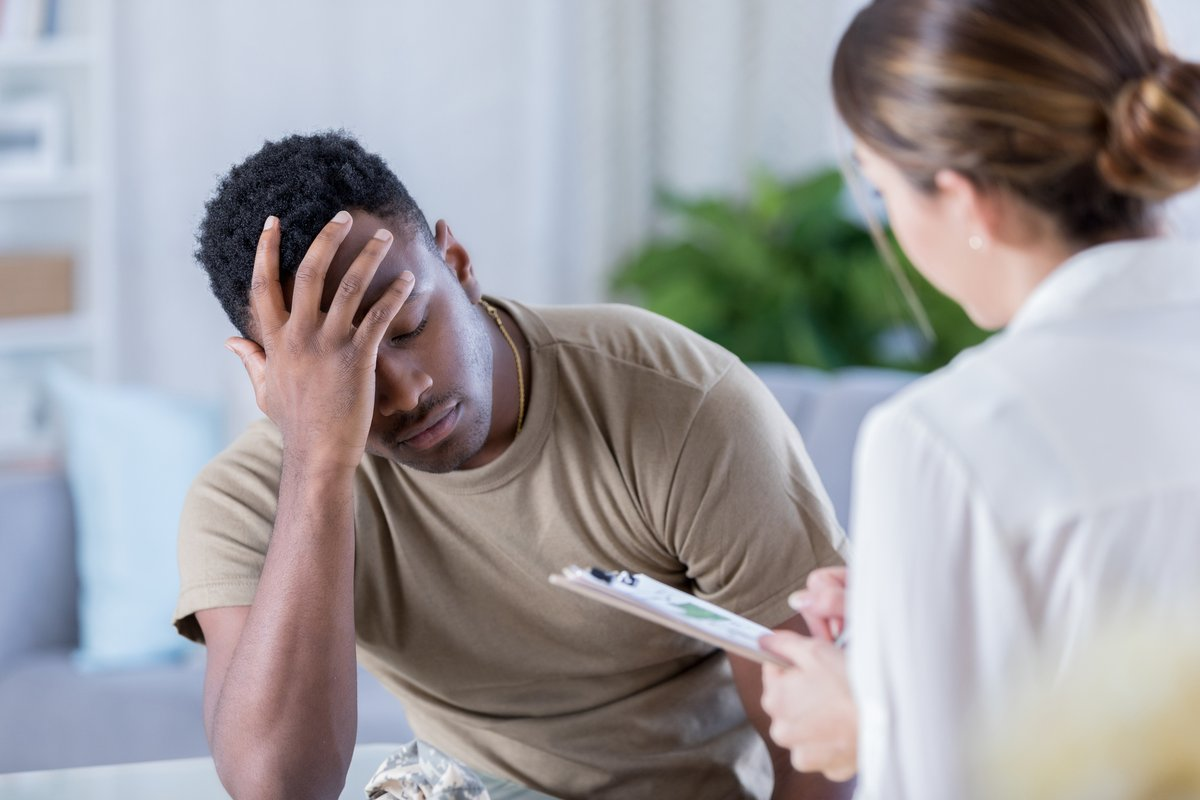
Psychiatric Comorbidities
Insomnia often happens with mental health issues like depression and anxiety disorders. This can make symptoms of both insomnia and mental health problems worse.
Research shows people with insomnia are more likely to get mental health issues. Treating both conditions together is often needed, making care more complex.
Medical Comorbidities
Insomnia is also linked to physical health problems, such as chronic pain, cardiovascular disease, and diabetes. The way insomnia and these conditions affect each other can impact treatment and outcomes.
The Bidirectional Relationship Between Insomnia and Other Disorders
The connection between insomnia and other health issues goes both ways. Insomnia can make other conditions worse, and vice versa. This shows the need for a complete care approach.
|
Comorbidity |
Effect on Insomnia |
Effect on Comorbidity |
|---|---|---|
|
Depression |
Increased severity of insomnia symptoms |
Worsening of depressive symptoms |
|
Chronic Pain |
Disrupted sleep patterns |
Increased pain perception |
|
Cardiovascular Disease |
Increased risk of cardiovascular events |
Potential worsening of cardiovascular health |
It’s vital to grasp these complex connections for effective treatment plans. By understanding how insomnia and other conditions interact, healthcare providers can offer better care.
Is Insomnia Truly a Disease? Examining the Evidence
Many sleep medicine experts are debating if insomnia disorder is a disease. We need to look at what makes a disease and how insomnia fits into this. This is key to understanding the issue.
Criteria for Disease Classification
To figure out if insomnia is a disease, we must know what a disease is. A disease has specific symptoms and changes that affect how our bodies work. It’s about knowing its cause, how it works, and how it shows up in people.
Criteria for a disease include:
- Specific diagnostic criteria
- Clear pathophysiological mechanisms
- Significant impact on quality of life or functional impairment
- Response to specific treatments
Insomnia as an Independent Pathological Entity
Insomnia disorder is now seen as a unique condition. Research shows it’s not just a symptom but a condition with its own causes. Studies have found brain changes and other factors that affect sleep.
Implications of Disease Status for Treatment and Research
If we see insomnia as a disease, it changes how we treat and study it. It could lead to better treatments and more research. This could also help with insurance coverage.
The table below shows what could change:
|
Aspect |
Disease Status |
Non-Disease Status |
|---|---|---|
|
Treatment Approach |
Specific treatments targeting insomnia pathology |
Symptom management as part of other conditions |
|
Research Focus |
In-depth studies on insomnia’s causes and mechanisms |
Limited research, considered secondary to other conditions |
|
Insurance Coverage |
Likely better coverage for insomnia-specific treatments |
Coverage may be limited or tied to other diagnoses |
The Debate Among Sleep Medicine Specialists
Even with growing evidence, experts keep debating if insomnia is a disease. Some say it’s too varied to be one disease. Others think its connection to other conditions makes it hard to classify.
This debate shows we need more research. As we learn more, how we see and treat insomnia might change.
The Long-term Health Consequences of Untreated Insomnia Disorder
Untreated insomnia can cause many health problems. It can affect your quality of life and overall well-being.
Physical Health Impacts
Insomnia can lead to serious physical issues. Cardiovascular disease is a big risk. It can cause high blood pressure, heart attacks, and strokes.
|
Physical Health Impact |
Description |
|---|---|
|
Cardiovascular Disease |
Increased risk of hypertension, heart attacks, and strokes. |
|
Weakened Immune System |
Reduced ability to fight off infections. |
|
Metabolic Changes |
Potential for weight gain or loss, and changes in appetite. |
Mental Health Consequences
Untreated insomnia also harms mental health. It can lead to or worsen mental health disorders like depression and anxiety.
“Sleep disturbance is a common symptom of many mental health disorders, and it can also be a contributing factor to the development of these disorders.”
Quality of Life and Functional Outcomes
Insomnia can greatly reduce your quality of life. It affects daily activities, work, and social interactions.
In conclusion, untreated insomnia has serious long-term effects. It harms physical health, mental well-being, and quality of life. Getting treatment early is key to avoiding these problems.
Treatment Approaches for Insomnia Disorder
Insomnia disorder treatment is complex and needs a personal touch. It involves several methods tailored to each person’s needs. A thorough check-up is key to understand the patient’s condition fully.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is a non-medical way to treat insomnia. It includes sleep hygiene, stimulus control, sleep restriction, and cognitive therapy. CBT-I focuses on changing the thoughts and behaviors that cause insomnia, helping improve sleep for the long term.
CBT-I teaches lasting sleep habits, not just quick fixes. Research shows it can greatly improve sleep quality and duration. These benefits last over time.
Pharmacological Interventions
Medications are used for short-term insomnia relief. Options include benzodiazepines, non-benzodiazepine hypnotics, and melatonin receptor agonists. Though meds offer quick relief, they’re not recommended for long-term use due to risks and side effects.
The right medication depends on several factors. These include the patient’s health history, insomnia severity, and other medication interactions. It’s important to consider the benefits and risks and monitor the patient closely.
Integrative and Complementary Approaches
Other methods like mindfulness meditation, yoga, acupuncture, and herbal supplements are also used. These can add benefits when used with traditional treatments.
Healthcare providers should talk about these options with patients. They should consider the evidence, possible interactions, and patient preferences when suggesting these therapies.
Conclusion: Recognizing Insomnia Disorder as a Serious Medical Condition
We’ve looked into insomnia disorder, a problem that affects many people around the world. It’s not just about not sleeping well. It’s a serious health issue that needs quick diagnosis and treatment to avoid long-term health problems.
It’s important to see insomnia disorder as a serious health issue. This helps us understand why we need to treat it well. Knowing how it works and its effects on our minds helps us find better ways to manage it.
There are good treatments out there, like cognitive behavioral therapy for insomnia (CBT-I) and medicines. By spreading the word about insomnia disorder and how to manage it, we can improve the lives of those who suffer from it.
As we learn more about insomnia disorder through research and reviews, we must recognize its serious nature. This way, we can offer better care and support to those who are struggling with it.
FAQ
What is insomnia disorder?
Insomnia disorder makes it hard to fall or stay asleep. It affects how well you function during the day.
Is insomnia a disease or a disorder?
Many see insomnia as both a disorder and a disease. It involves complex issues and can harm health.
What are the symptoms of insomnia disorder?
Symptoms include trouble falling or staying asleep. You might wake up too early. Daytime problems like tiredness and mood issues also occur.
How is insomnia disorder diagnosed?
Doctors use a detailed sleep history to diagnose. They might also look at criteria from the DSM-5 or ICD-11.
What is the prevalence of insomnia disorder?
Many adults worldwide have insomnia disorder. The exact number varies based on the criteria used and the population studied.
What are the comorbidities associated with insomnia disorder?
Insomnia often goes hand-in-hand with depression, anxiety, chronic pain, and heart disease.
How does insomnia disorder impact daily life?
It can really affect your daily life. It might hurt your work, social life, and overall happiness.
What are the treatment options for insomnia disorder?
Treatments include Cognitive Behavioral Therapy for Insomnia (CBT-I), medicines, and other therapies.
Is insomnia disorder a serious medical condition?
Yes, it’s considered serious. It can harm your health and quality of life if not treated.
Can insomnia disorder be considered a pathology?
Yes, it involves serious underlying issues. These include hyperarousal and changes in the brain.
What are the long-term health consequences of untreated insomnia disorder?
If left untreated, it can lead to serious health problems. This includes a higher risk of chronic diseases and other issues.
How does the classification of insomnia disorder impact treatment?
How we classify it affects treatment. It influences the therapies used and how severe the condition is seen.
References
National Center for Biotechnology Information. Insomnia Disorder: Symptoms, Pathology, and Disease Classification. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33985347/