Stem cells can develop into many cell types and act as the body’s repair system. They replace or restore damaged tissues, offering new possibilities for treating diseases.
Send us all your questions or requests, and our expert team will assist you.

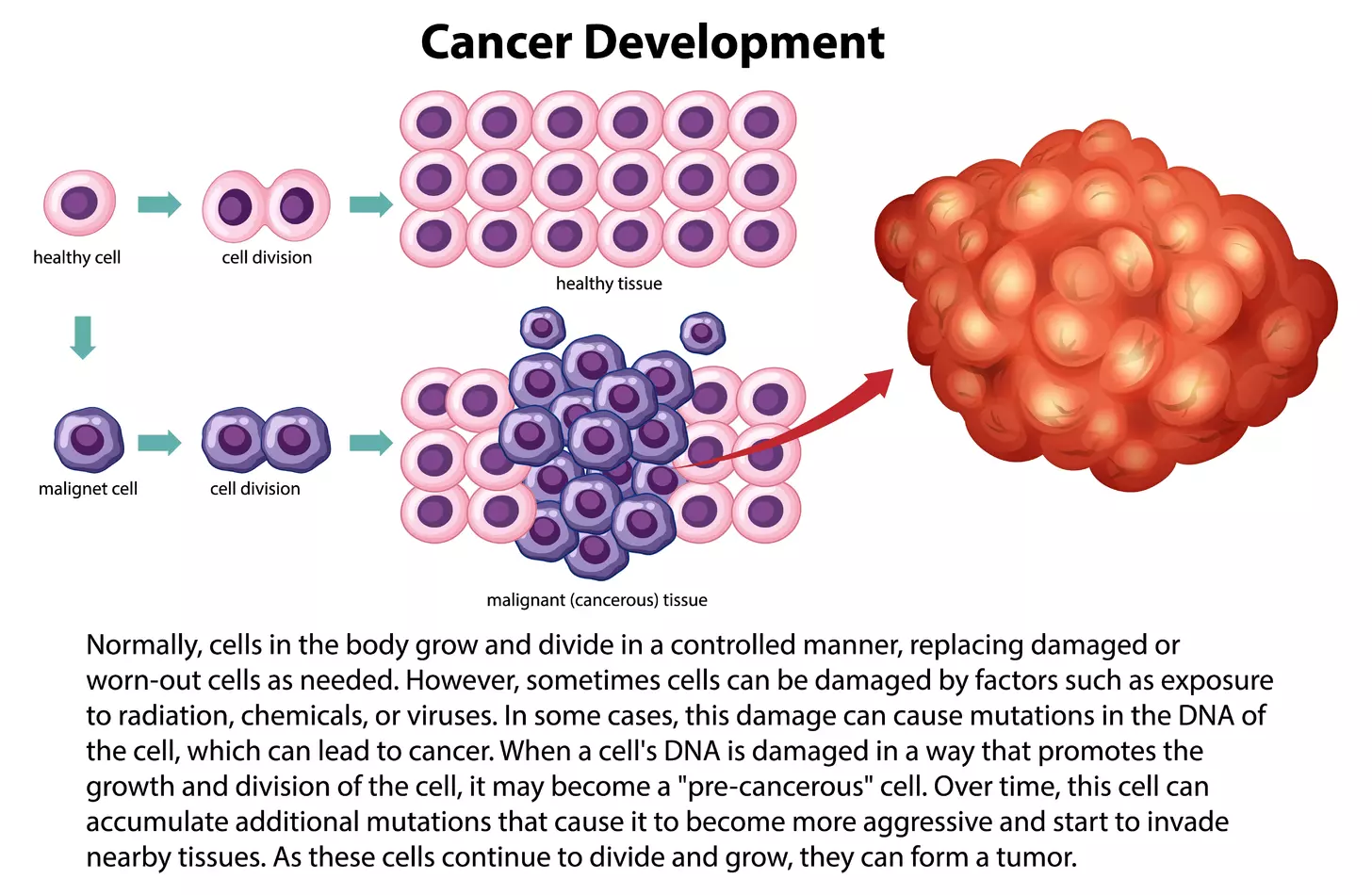
Diagnosing lymphoma is a careful process that involves a team of specialists. It is not just about finding cancer, but also about identifying the exact type, its genetic features, and the patient’s overall strength. This detailed approach is necessary because treatments are now highly personalized. The results of this evaluation help doctors decide on the best therapy, whether it is standard chemotherapy, targeted drugs, or advanced treatments like stem cell transplants.

The diagnostic journey typically begins with a clinical assessment. A physician performs a comprehensive physical examination, palpating the nodal basins in the neck (cervical), above the collarbone (supraclavicular), armpits (axillary), and groin (inguinal). The character of the lymph nodes is noted; malignant nodes are often described as firm, rubbery, and painless, whereas nodes swollen due to infection are usually tender and soft. The physician also palpates the abdomen to assess for splenomegaly (enlarged spleen) or hepatomegaly (enlarged liver), as the lymphatic system is integrated with these organs. A thorough review of systems is conducted to identify B-symptoms and other indicators such as fatigue, pruritus (severe itching), or early satiety.

No diagnosis of lymphoma can be confirmed without a tissue biopsy. Blood tests alone are insufficient. The architecture of the lymph node and the pattern of cell distribution are critical for accurate subtyping.

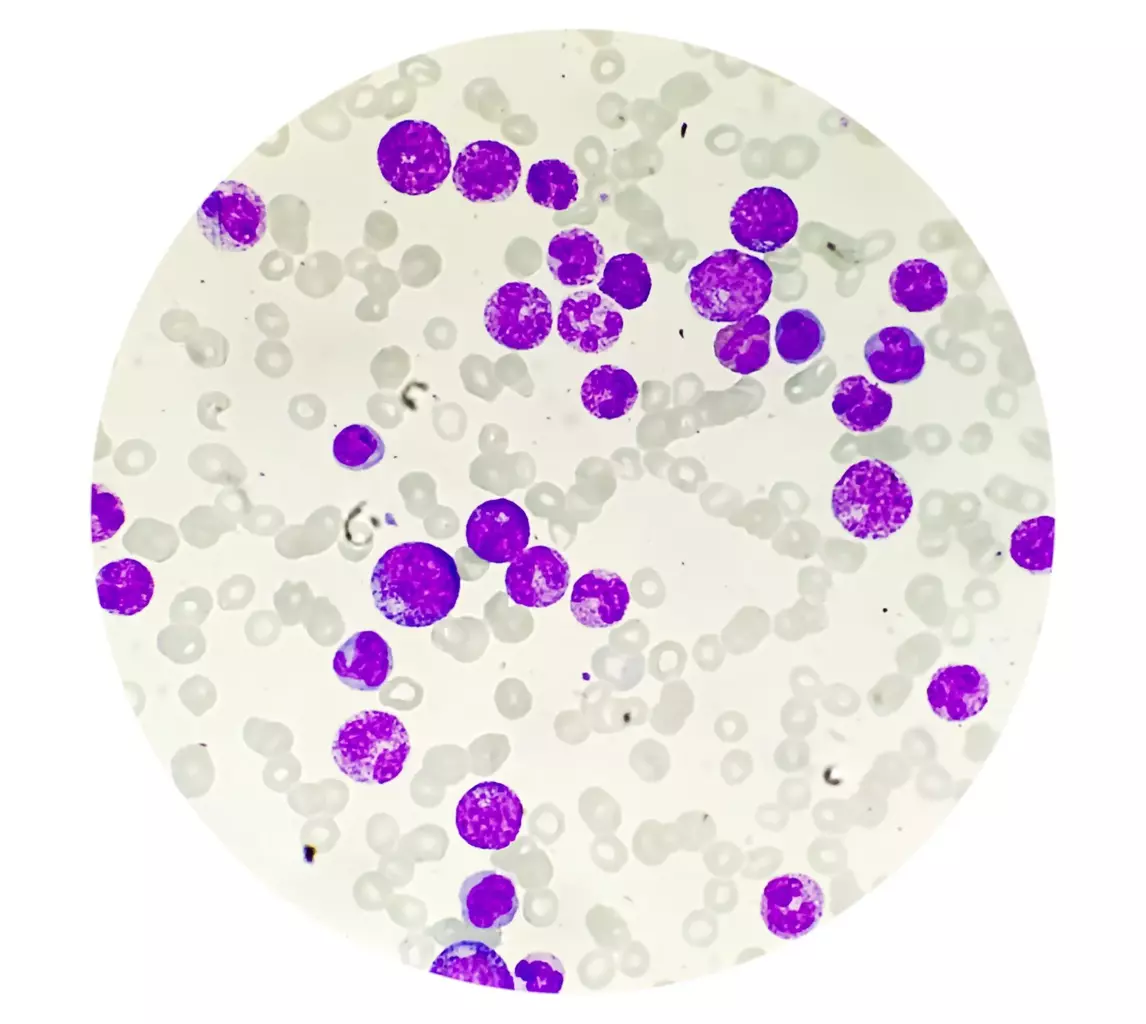
Once tissue is obtained, it undergoes sophisticated analysis in the pathology laboratory. This is where the specific identity of the lymphoma is revealed.

To determine the stage of the disease, physicians must visualize the body’s internal landscape.

Since lymphoma is a disease of the blood system, evaluating the “factory” is often necessary. A bone marrow aspiration and biopsy involves inserting a needle into the pelvic bone to withdraw liquid marrow and a small core of bone tissue. This sample is examined to determine if lymphoma cells have infiltrated the marrow. Marrow involvement typically classifies the disease as Stage IV. However, with the high sensitivity of PET/CT scans, the need for bone marrow biopsies is being re-evaluated for specific subtypes, such as Hodgkin Lymphoma, though it remains standard for many Non-Hodgkin Lymphomas and is a prerequisite for any patient considered for autologous stem cell harvesting.

Before initiating intensive treatments, especially regimens involving stem cell transplantation or anthracycline-based chemotherapy, the patient’s organ function must be evaluated to ensure they can withstand the physiological stress.
Send us all your questions or requests, and our expert team will assist you.
Lymphoma diagnosis relies not only on identifying abnormal cells but also on assessing how those cells are arranged within the lymph node. FNA only sucks out loose cells, destroying the “architecture” of the tissue. Without seeing the pattern (follicular vs. diffuse), pathologists cannot accurately determine the specific lymphoma subtype.
The level of radiation exposure from a PET/CT scan is generally considered safe and the diagnostic value it provides is immense. The radioactive tracer has a very short half-life and decays rapidly, usually leaving the body within a day. The benefits of accurately staging the cancer far outweigh the minimal risk associated with the radiation.
Staging determines the location and extent of the cancer in the body. It tells the medical team whether the lymphoma is localized to one area (early stage) or has spread to multiple lymph node regions or organs (advanced stage). This directly dictates the type and duration of treatment required.
The procedure is performed with local anesthesia to numb the skin and the surface of the bone. While patients may feel pressure and a brief, sharp sensation when the marrow is withdrawn, it is generally well-tolerated. Sedation can also be offered to minimize anxiety and discomfort during the procedure.
Preliminary pathology results might be available within 2 to 3 days, but the final report—which includes complex immunohistochemistry and molecular genetic testing—can take 5 to 10 days. This waiting period is critical to ensure the diagnosis is as precise as possible before starting a treatment plan.






Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)