Stem cells can develop into many cell types and act as the body’s repair system. They replace or restore damaged tissues, offering new possibilities for treating diseases.
Send us all your questions or requests, and our expert team will assist you.

The treatment of lymphoma has evolved into a sophisticated, multimodal discipline. The strategy is highly personalized and depends on the specific subtype (Hodgkin vs. Non-Hodgkin), the stage of disease, the patient’s age, and their overall physiological fitness. The therapeutic arsenal ranges from conventional chemotherapy and radiation to cutting-edge immunotherapy and regenerative cellular therapies. For many patients, the goal is curative; for others with indolent forms, the goal is long-term disease control and preservation of quality of life.

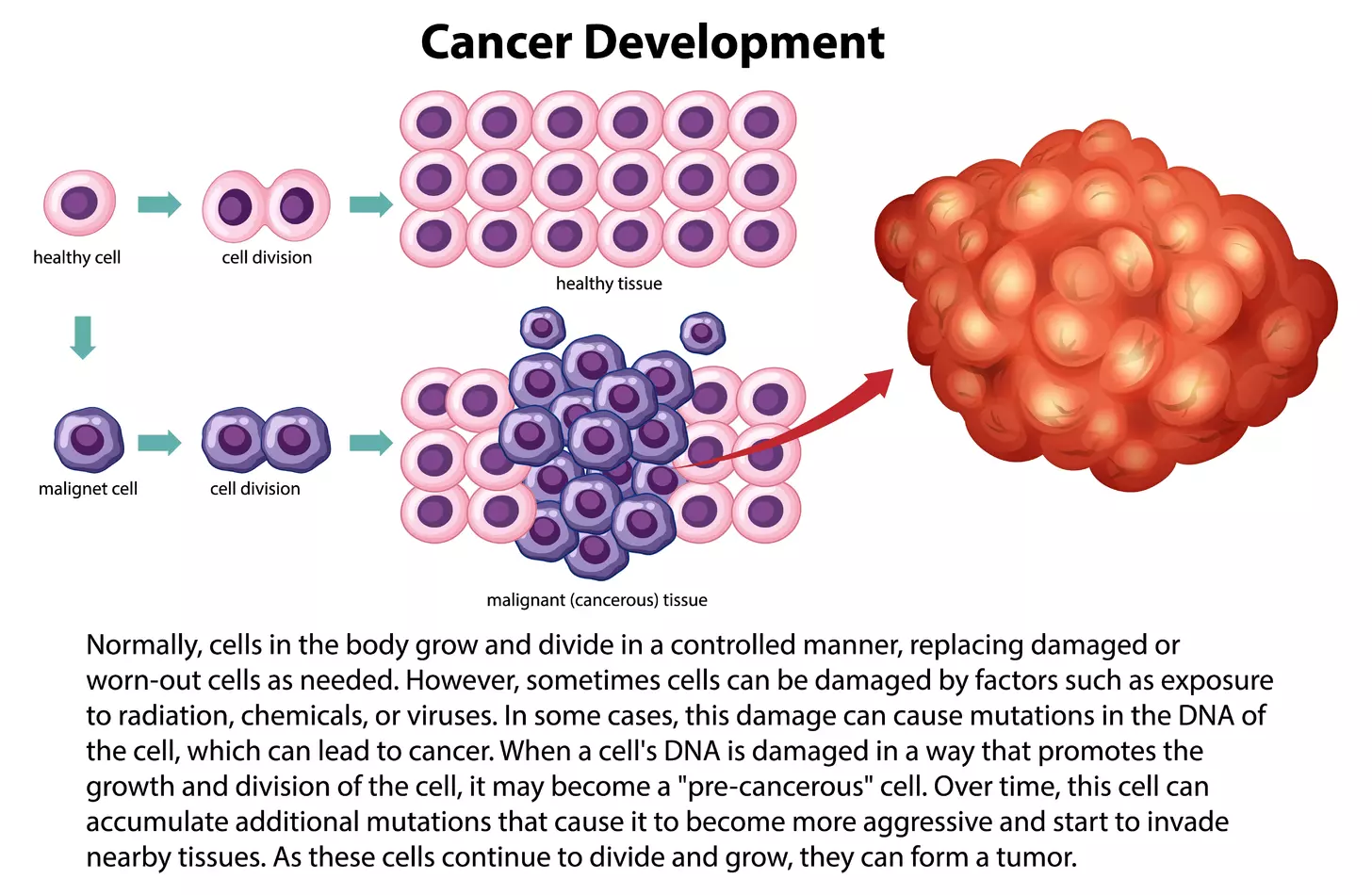
Chemotherapy remains the backbone of treatment for most aggressive lymphomas. These systemic drugs travel through the bloodstream to reach cancer cells throughout the lymphatic system and organs.

This category of treatment represents a shift away from “carpet-bombing” chemotherapy toward precision medicine. These drugs target specific proteins or pathways that lymphoma cells use to survive.

Modern radiation therapy is highly focused. It uses high-energy rays to destroy cancer cells in a specific area. It is often used as a consolidation therapy after chemotherapy to eliminate any residual disease in sites that were originally bulky. Advanced techniques like Involved Site Radiation Therapy (ISRT) use computer planning to shape the radiation beam, sparing surrounding healthy organs, such as the heart and lungs, from unnecessary exposure.

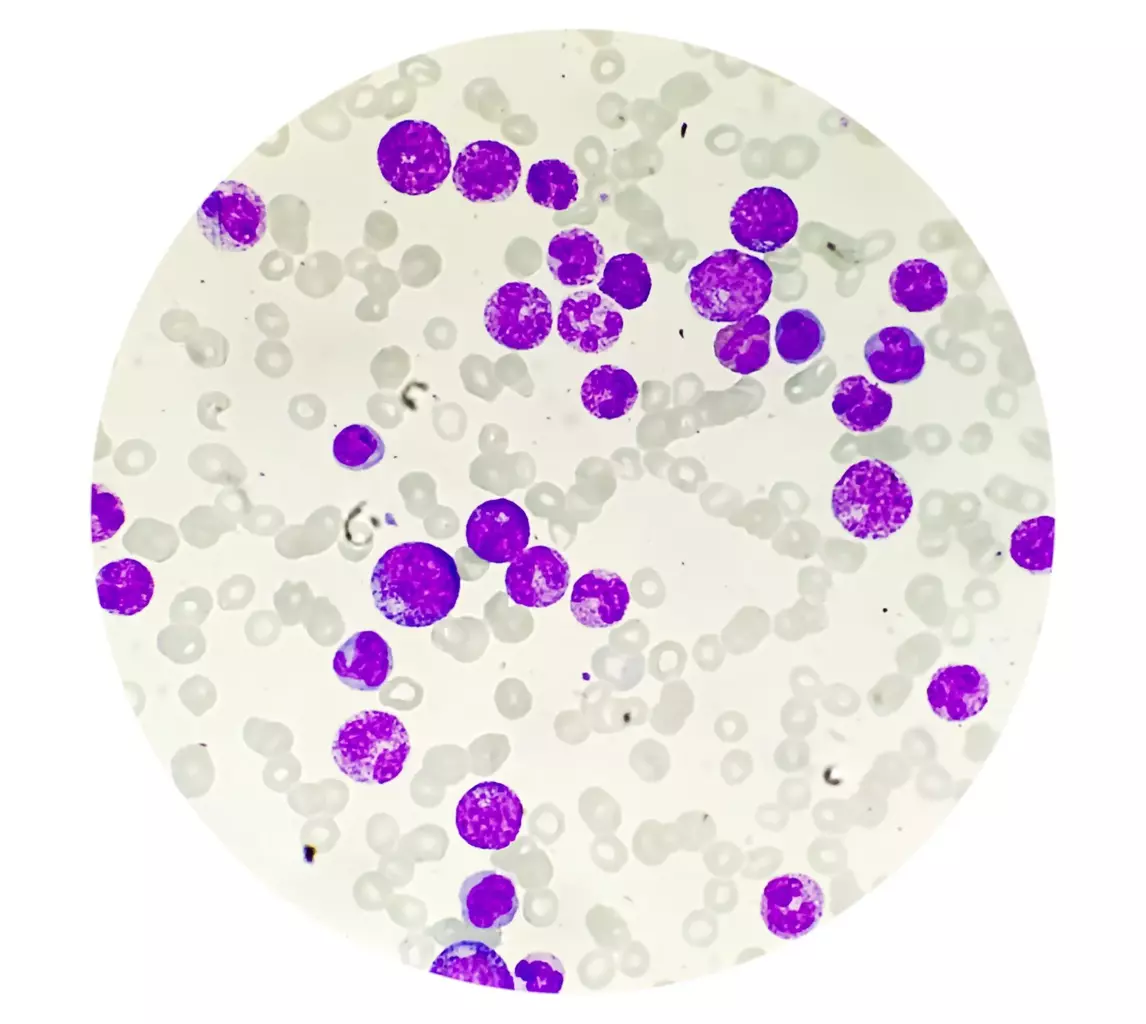
For patients with high-risk, relapsed, or refractory lymphoma, standard chemotherapy may be insufficient. In these cases, stem cell transplantation is a critical, potentially curative intervention. This procedure relies on the regenerative capacity of hematopoietic stem cells to restore bone marrow function.

This procedure uses the patient’s own stem cells. It is the most common transplant type for lymphoma.

This procedure uses stem cells from a donor (sibling, matched unrelated donor, or haploidentical relative).

Chimeric Antigen Receptor (CAR) T-cell therapy is a groundbreaking cellular gene therapy. It involves collecting the patient’s own T cells, genetically engineering them in a laboratory to express a receptor that targets a specific protein on the lymphoma cell (usually CD19), expanding them into millions of cells, and infusing them back into the patient. These “living drugs” circulate in the body, actively hunting and destroying lymphoma cells. This therapy is currently approved for certain relapsed B-cell lymphomas and represents the frontier of regenerative immunotherapy.

Managing the side effects of these intensive treatments is integral to the procedure.
Send us all your questions or requests, and our expert team will assist you.
An autologous transplant uses your own stem cells to rescue your bone marrow after high-dose chemotherapy. An allogeneic transplant uses donor stem cells. The donor transplant provides a new immune system that can fight the cancer (Graft-versus-Lymphoma effect) but carries higher risks of immunological complications like Graft-Versus-Host Disease.
Many chemotherapy regimens used for lymphoma, such as R-CHOP or ABVD, do cause temporary hair loss (alopecia). However, not all treatments have this side effect. Some targeted therapies and immunotherapies may not cause significant hair loss. Hair typically begins to regrow 3 to 6 months after treatment concludes.
Conditioning refers to the high-dose chemotherapy and/or total-body irradiation administered to the patient immediately before the stem cell infusion. The purpose is twofold: to eliminate as many lymphoma cells as possible and to suppress the patient’s immune system (in allogeneic transplants) so it does not reject the new donor cells.
A stem cell transplant replaces the blood-forming system (bone marrow). CAR-T therapy modifies specific immune cells (T-cells) to recognize cancer. CAR-T does not replace the bone marrow but instead introduces a genetically modified “hunter” cell to the existing immune system. It is often used when transplants have failed or are not an option.
No, the actual delivery of radiation is painless, similar to getting an X-ray. Patients cannot feel the radiation entering their bodies. However, side effects such as skin irritation (like a sunburn) or fatigue may develop gradually over the course of treatment.






Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)