Asking what does it mean if u cough up blood? Learn the urgent causes and when to seek immediate medical help for bleeding.
Coughing up blood in phlegm, known as hemoptysis, can be scary. But, in about 95% of cases, the bleeding stops by itself and isn’t serious. At Liv Hospital, we know finding out why it happens is key to the right treatment.
We’ll look at why hemoptysis happens, from mild to serious reasons. Knowing when to see a doctor is important for your lungs. Our care focuses on you, using global medical standards to help you understand your symptoms. This helps figure out if you need to see a doctor right away.
Key Takeaways
- Hemoptysis is the medical term for coughing up blood from the respiratory tract.
- In most cases, bleeding stops on its own and is not severe.
- Understanding the underlying cause is vital for proper care.
- Various conditions can cause hemoptysis, ranging from mild to severe.
- Seeking medical attention is necessary if you experience persistent or severe symptoms.
What Does It Mean If U Cough Up Blood?

Coughing up blood can be scary. It’s important to know what it means. This symptom, called hemoptysis, can show many health problems, from mild to serious.
Definition of Hemoptysis
Hemoptysis means coughing up blood or blood-stained mucus. It can happen for many reasons, like infections or lung cancer. Knowing what hemoptysis is helps you understand why it’s a concern.
“Hemoptysis is a symptom that warrants medical evaluation to determine its cause and appropriate treatment.”
How Common Is This Condition?
Hemoptysis is not rare. It can happen to people with many respiratory issues. While it’s often linked to serious diseases, sometimes the bleeding is not bad and stops by itself. But, ignoring this symptom is not wise, as it might signal a serious health issue.
The 95/5 Rule: Understanding the Statistics
The “95/5 rule” explains hemoptysis. It says 95% of cases are not serious, with mild bleeding. But, 5% can be very dangerous, with heavy bleeding that might block airways. Knowing this can help you feel better, but always see a doctor.
Even though most hemoptysis cases are not severe, it’s always a sign to see a doctor. They can figure out the cause and how to treat it.
Identifying Blood in Phlegm: Appearance and Characteristics

Coughing up blood in phlegm can be scary. It’s important to know what it looks like. This helps figure out why it’s happening and what to do next.
Different Presentations: Streaks, Specks, and Clots
Blood in phlegm can show up in different ways. You might see streaks, specks, or even clots. Streaky blood in phlegm is common, with thin blood strands mixed with mucus. Sometimes, you’ll see small specks, and in severe cases, clots.
Colors and Textures to Look For
The color and texture of blood in phlegm are clues. Fresh blood is bright red, while older blood looks rust-colored or brown. The texture can be thin and watery or thick and sticky, depending on the mucus.
Differentiating Blood in Phlegm from Other Substances
It’s not easy to tell if it’s blood in phlegm. Foods or meds can make phlegm look bloody. We need to tell true blood from other things that look like it. Getting it right is important for the right treatment.
In short, knowing what blood in phlegm looks like is key. By spotting the different looks, colors, and textures, and telling it apart from other things, we can take the right steps towards diagnosis and care.
Common Respiratory Infections Causing Blood in Phlegm
Blood in phlegm can come from many respiratory infections. It’s key to find out why. These infections can make airways inflamed and irritated, causing blood in phlegm. We’ll look at how acute bronchitis and pneumonia can lead to this symptom.
Acute Bronchitis
Acute bronchitis is a common infection that can cause blood in phlegm. It makes the bronchial tubes inflamed, often from a virus. The coughing from bronchitis can irritate the airways, leading to blood in phlegm.
In most cases, it gets better on its own. But, it’s important to watch symptoms to make sure they don’t get worse.
Pneumonia
Pneumonia is a serious infection that can also cause hemoptysis. It makes the lung tissue inflamed, often from bacteria, viruses, or fungi. This can fill the lung’s air sacs with fluid, causing coughing, fever, and trouble breathing.
When coughing, blood in phlegm can appear due to lung tissue damage and inflammation.
Blood in Phlegm After Flu or Cold
It’s common to see blood in phlegm after a flu or cold. The coughing from these infections can irritate airways and damage small blood vessels, causing hemoptysis. While it might seem scary, it often goes away as the infection clears.
But, if it doesn’t go away, seeing a doctor is a good idea. They can check for any other issues that might need treatment.
Knowing why blood in phlegm happens after respiratory infections helps us take the right steps. If you’ve coughed up a little blood in phlegm after a flu or cold, watching your symptoms and seeing a doctor if they don’t get better is wise.
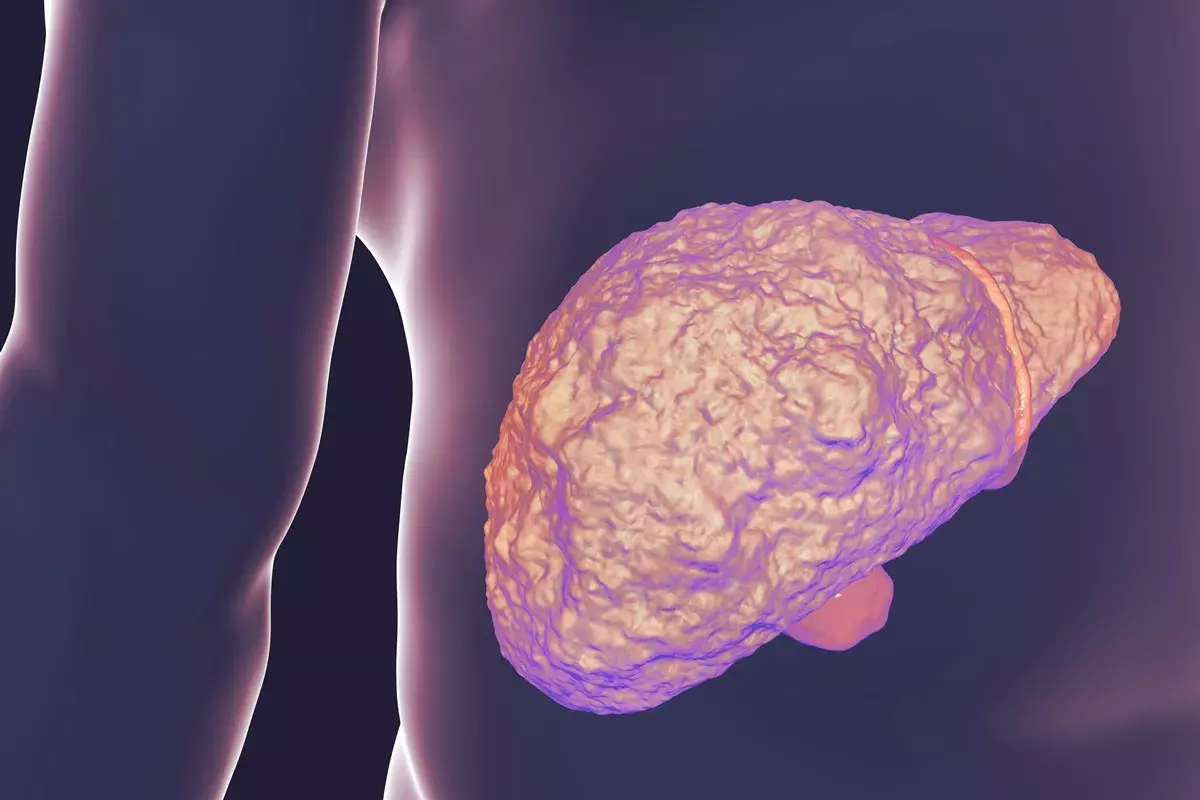
Chronic Conditions Associated with Hemoptysis
Chronic respiratory diseases can cause hemoptysis, where patients cough up blood or blood-stained mucus. It’s key to understand these conditions to manage symptoms and avoid complications.
Tuberculosis
Tuberculosis (TB) is a serious lung disease. TB can damage lung tissue a lot, leading to hemoptysis. Coughing up blood is a symptom in TB’s advanced stages, due to cavitation or inflammation.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is a lung disease that gets worse over time. It’s mainly caused by smoking, but also by genetics and environment. COPD can cause chronic bronchitis and emphysema, raising the risk of hemoptysis due to airway damage.
Bronchiectasis
Bronchiectasis makes the airways of the lungs wider than normal. This leads to chronic infections and inflammation. The damage can cause persistent coughing and potentially hemoptysis due to blood vessel erosion.
Cystic Fibrosis
Cystic fibrosis is a genetic disorder that severely damages lungs, digestive system, and other organs. It causes thick, sticky mucus that clogs airways and traps bacteria. This leads to infections, inflammation, and severe complications like hemoptysis.
Managing respiratory health is vital to prevent hemoptysis and other complications. Regular doctor visits and following treatment plans can greatly reduce severe symptom risks.
Serious Medical Concerns: When Blood in Phlegm Signals Danger
Hemoptysis, or coughing up blood, is a symptom that needs quick attention. It can be linked to serious health issues. While many causes are not dangerous, some serious conditions can show up with this symptom.
Lung Cancer
Lung cancer is a major worry with hemoptysis. Coughing up blood or bloody mucus can be a sign of lung cancer, mainly in later stages.
We will talk about why early detection is key. We will also look at the treatment options for lung cancer patients.
Pulmonary Embolism
A pulmonary embolism happens when a blood clot blocks a lung blood vessel. This can cause hemoptysis. It’s a serious condition that needs quick medical help.
Recognizing the signs of a pulmonary embolism, like sudden shortness of breath or chest pain, is vital for timely treatment.
Pulmonary Edema
Pulmonary edema is when fluid builds up in the lungs, leading to coughing up blood. It often comes from heart failure or other heart problems.
It’s important to know what causes pulmonary edema to manage it well.
Autoimmune Conditions Affecting the Lungs
Certain autoimmune diseases, like Goodpasture syndrome or vasculitis, can harm the lungs and cause hemoptysis. These conditions need special treatment to control symptoms and avoid further problems.
We will look at the different autoimmune conditions that can affect the lungs. We will also see why getting an accurate diagnosis is so important.
In conclusion, while blood in phlegm can have many causes, it’s key to know the serious health concerns it can signal. If you’re coughing up blood a lot or it’s severe, you should see a doctor right away.
Cardiovascular Causes of Coughing Up Blood
Hemoptysis, or coughing up blood, can be caused by heart and blood vessel problems. These issues need quick medical help. They can cause bleeding in the lungs due to heart or blood vessel issues.
Congestive Heart Failure
Congestive heart failure (CHF) means the heart can’t pump enough blood. This leads to fluid in the lungs, called pulmonary congestion. This can cause coughing up blood.
In CHF, high pressure in the lungs’ veins can leak fluid into airspaces. This results in hemoptysis.
Key aspects of CHF that contribute to hemoptysis include:
- Increased pulmonary venous pressure
- Fluid overload
- Potential for pulmonary edema
Mitral Valve Stenosis
Mitral valve stenosis narrows the mitral valve opening. This blocks blood flow from the left atrium to the left ventricle. It can cause high pressure in the left atrium and lungs, leading to hemoptysis.
|
Condition |
Effect on Pulmonary System |
Risk of Hemoptysis |
|---|---|---|
|
Mitral Valve Stenosis |
Increased pulmonary venous pressure |
Moderate to High |
|
Congestive Heart Failure |
Pulmonary congestion and edema |
High |
|
Arteriovenous Malformations |
Abnormal connections between arteries and veins |
High |
Arteriovenous Malformations
Arteriovenous malformations (AVMs) are abnormal connections between arteries and veins. In the lungs, they can cause hemoptysis because these vessels are fragile. AVMs can rupture, leading to significant bleeding.
It’s important to understand these cardiovascular causes of hemoptysis. Each condition needs a specific treatment plan to manage coughing up blood.
When to Seek Medical Attention for Blood in Phlegm
Blood in phlegm can be scary. It’s key to know when you need to see a doctor right away. We’ll show you the signs that mean you should get medical help and what to expect at your visit.
Emergency Warning Signs
If you notice any of these symptoms, get medical help fast:
- Coughing up large amounts of blood: If you cough up more than a couple of tablespoons, it’s a big emergency.
- Chest pain or tightness: Chest pain or discomfort could mean a serious problem.
- Difficulty breathing: Trouble breathing or feeling short of breath is a serious sign.
- Severe dizziness or fainting: Dizziness or fainting can mean you’ve lost a lot of blood or have a serious issue.
Non-Emergency Situations That Warrant a Doctor’s Visit
Even without emergency signs, see a doctor if you have:
- Persistent coughing up blood: If you keep coughing up blood or blood-tinged phlegm for days.
- Recurring episodes: If you keep having episodes of coughing up blood.
- Underlying health conditions: If you have health issues like heart or lung disease.
|
Situation |
Recommended Action |
|---|---|
|
Coughing up blood with no other symptoms |
Schedule a doctor’s visit within a few days |
|
Experiencing chest pain or difficulty breathing |
Seek immediate medical attention |
|
Having a persistent cough with blood-tinged phlegm |
Consult a doctor within a week |
What Information to Prepare for Your Healthcare Provider
To help your doctor, prepare this information:
- Detailed medical history: Share your medical history, including any health conditions you have.
- Symptoms and duration: Tell your doctor about your symptoms, when they started, and how long they’ve lasted.
- Medications and supplements: List any medicines or supplements you’re taking.
“Accurate diagnosis relies heavily on the information provided by the patient. Being prepared with your medical history and symptoms can significantly impact the effectiveness of your treatment plan.” – Medical Expert, Pulmonologist
Knowing when to get medical help for blood in phlegm and being ready for your doctor’s visit is key. This way, you’ll get the right care for your condition.
Diagnosis and Treatment Approaches
Diagnosing hemoptysis involves several steps and tests. These tests help find the cause of the bleeding. Knowing the cause is key to choosing the right treatment.
Common Diagnostic Tests
We use many tests to find the cause of hemoptysis. These include:
- Chest X-rays: A chest X-ray is often the first imaging test performed to look for abnormalities in the lungs.
- CT Scans: Computed Tomography (CT) scans provide more detailed images of the lungs and can help identify the source of bleeding.
- Bronchoscopy: This procedure involves inserting a flexible tube with a camera into the airways to visually inspect the lungs and air passages.
These tests help us find the cause of hemoptysis. It could be an infection or something more serious like lung cancer.
Treatment Strategies Based on Underlying Causes
Treatment for hemoptysis varies based on the cause. For example:
- Infections: If the cause is an infection, treatment may involve antibiotics or antiviral medications.
- Chronic Conditions: For chronic conditions like COPD or bronchiectasis, treatment focuses on managing symptoms and preventing exacerbations.
- Surgical Interventions: In some cases, surgical intervention may be necessary to address the underlying cause, such as removing a tumor or repairing vascular malformations.
Home Management Techniques
While getting treatment, there are ways to manage symptoms at home. These include:
- Stay Hydrated: Drinking plenty of fluids can help thin out mucus and keep the airways moist.
- Use a Humidifier: Adding moisture to the air can help soothe the airways and reduce coughing.
- Avoid Irritants: Stay away from smoke, dust, and other pollutants that can irritate the lungs.
Understanding the cause of hemoptysis and using the right treatments can help manage the condition. This approach improves patient outcomes.
Conclusion
Coughing up blood in phlegm, or hemoptysis, is a symptom that needs attention. We’ve looked at many causes, from mild infections to serious diseases like lung cancer and pulmonary embolism.
It’s important to understand the causes and when to see a doctor. We’ve talked about how doctors diagnose and treat this condition.
In short, hemoptysis is a complex issue with many possible reasons. Being informed and getting medical help when needed is key. This way, people can manage their condition well and avoid serious problems. Our discussion ends by stressing the need for quick medical check-ups for the right diagnosis and treatment.
FAQ
What is hemoptysis?
Hemoptysis is when you cough up blood or bloody mucus from your lungs or airways. It can be mild or very serious. You should see a doctor if you have it.
Is coughing up blood always a sign of a serious condition?
No, it’s not always serious. Most of the time, the bleeding stops on its own. But, you should find out why it happened to know what to do next.
What are the common causes of blood in phlegm?
Blood in phlegm can come from many things. It might be from infections like bronchitis or pneumonia. Or it could be from long-term conditions like COPD or cystic fibrosis. Even heart problems can cause it.
Can a cold or flu cause blood in phlegm?
Yes, a cold or flu can make you cough up blood. This is because coughing can irritate your airways and cause bleeding.
What does blood in phlegm look like?
Blood in phlegm can look like streaks, specks, or clots. It can be bright red, rust-colored, or pink. It might be mixed with mucus or look like separate blood clots.
When should I seek medical attention for blood in phlegm?
You need to see a doctor right away if you cough up a lot of blood. Or if you have trouble breathing, chest pain, or if the blood is frothy or pink. Even if it’s not that bad, it’s good to get checked out.
How is the cause of hemoptysis diagnosed?
Doctors use tests like chest X-rays and CT scans to find out why you’re coughing up blood. They might also do a bronchoscopy or blood tests.
What are the treatment strategies for hemoptysis?
Treatment depends on why you’re coughing up blood. It could be just taking medicine at home or needing to stay in the hospital. Doctors might do procedures or surgery to stop the bleeding.
Can I manage blood in phlegm at home?
If it’s just a little blood, you can try to manage it at home. Drink lots of water, use a humidifier, and avoid smoke. But, you should see a doctor to make sure it’s okay.
Is it normal to cough up blood in the morning?
Coughing up blood in the morning might mean you have an infection like bronchitis. It’s not always serious, but it’s good to talk to a doctor about it.
Can cardiovascular conditions cause hemoptysis?
Yes, heart problems like congestive heart failure or mitral valve stenosis can cause you to cough up blood. It’s important to manage these conditions to avoid worse problems.
References
World Health Organization. Hemoptysis: Causes, Severity, and Treatment Considerations. Retrieved from https://www.who.int/news-room/fact-sheets/detail/tuberculosis