Angiopathy comes from Greek words meaning “disease of blood vessels.” It’s a big health issue that affects many parts of our blood vessels. It includes both arteries and veins. It’s split into macroangiopathy and microangiopathy, showing a wide range of blood vessel problems what is angiopathy.
Angiopathy means disease or damage to blood vessels. This can cause many problems, like those seen in diabetes and amyloid deposits. Knowing about angiopathic conditions is key to managing and treating them well.
Key Takeaways
- Angiopathy refers to disease or damage to blood vessels.
- It affects both arteries and veins.
- Macroangiopathy and microangiopathy are the two main classifications.
- Diabetes and amyloid deposits are common causes.
- Effective management requires understanding angiopathic conditions.
What Is Angiopathy: Definition and Medical Significance

Understanding angiopathy is key to diagnosing and treating vascular diseases. Angiopathy is a disease of blood vessels. It can cause different problems depending on the affected vessels and organs.
The term angiopathy comes from Greek. “Angio-” means vessel, and “-pathy” means disease or suffering. This helps us see how it affects blood vessel health.
Etymology and Medical Terminology
In medical terms, angiopathy describes various vascular disorders. It can affect both arteries and veins, showing different symptoms.
Studying angiopathy means looking at how blood vessels work, their diseases, and how they relate to medicine. Macroangiopathy, for example, is a disease of big blood vessels. It can cause serious heart problems.
Historical Context in Vascular Medicine
Our understanding of angiopathy has grown a lot with advances in vascular medicine. Early studies of vascular diseases helped create today’s treatments.
As science improved, we’ve learned more about different types of angiopathy. This includes diabetic angiopathy and cerebral amyloid angiopathy (CAA).
Global Prevalence and Impact
Angiopathic diseases are a big health problem worldwide. Studies show they’re becoming more common, mainly in people with diabetes and high blood pressure.
|
Condition |
Prevalence |
Impact |
|---|---|---|
|
Diabetic Angiopathy |
High in diabetic populations |
Increased risk of cardiovascular events and renal failure |
|
Cerebral Amyloid Angiopathy (CAA) |
Common in elderly populations |
Associated with cognitive decline and stroke |
|
Macroangiopathy |
Prevalent in populations with hypertension and atherosclerosis |
Increased risk of myocardial infarction and peripheral artery disease |
The worldwide effect of angiopathy shows we need more research and better ways to manage it. This is to protect public health.
The Pathophysiology of Angiopathic Disease
Angiopathic disease is a complex condition that affects blood vessels. It involves damage and dysfunction in these vessels. This damage can lead to serious health issues.
Normal Blood Vessel Structure and Function
Blood vessels have three main layers: the tunica intima, tunica media, and tunica externa. The tunica intima is the innermost layer, lined with endothelial cells. The tunica media, in the middle, contains smooth muscle cells and elastic fibers. The outermost layer, the tunica externa, is made of connective tissue.
Blood vessels are vital for maintaining balance in the body. They help control blood pressure and flow. Endothelial cells play a key role in this, producing substances that affect blood flow and clotting.
Mechanisms of Vascular Damage and Dysfunction
Angiopathic disease damages blood vessels through inflammation, oxidative stress, and shear stress. These factors can cause the endothelium to malfunction. This imbalance affects blood flow and vessel function.
- Inflammation: Inflammatory cells and cytokines damage vessels.
- Oxidative Stress: ROS can harm cells and disrupt vessel function.
- Shear Stress: Unusual blood flow patterns can harm endothelial cells.
Cellular and Molecular Changes in Angiopathy
At a cellular and molecular level, angiopathy involves changes in gene expression and signaling pathways. For example, hyperglycemia in diabetes activates pathways that produce AGEs. These AGEs accumulate in vessels and cause damage.
|
Pathway |
Description |
Effect on Blood Vessels |
|---|---|---|
|
AGEs Formation |
Accumulation of advanced glycosylation end-products |
Vessel wall damage and stiffness |
|
Oxidative Stress |
Production of reactive oxygen species |
Endothelial dysfunction and vascular inflammation |
|
Inflammatory Response |
Recruitment of inflammatory cells and release of cytokines |
Vascular damage and atherosclerosis |
Diabetic angiopathy is a common form of angiopathic disease. Understanding its mechanisms is key to finding effective treatments.
Risk Factors and Causes of Angiopathy
Angiopathy comes from a mix of genetics, lifestyle, and environment. Knowing these factors helps prevent and manage angiopathic conditions.
Genetic Predisposition
Genetics play a big role in getting angiopathy. People with a family history of vascular diseases are at higher risk. Studies have found genetic markers linked to diabetic angiopathy and other types.
“Genetic predisposition is a critical factor in the development of angiopathy, highlighting the need for early screening and preventive measures in high-risk populations.”
Medical Expert, Vascular Specialist
Lifestyle Factors
Our lifestyle choices affect our risk of getting angiopathy. Smoking, not moving much, and eating too much fat harm our blood vessels. Stopping smoking and eating more fruits, veggies, and whole grains can help.
|
Lifestyle Factor |
Impact on Angiopathy Risk |
|---|---|
|
Smoking |
Increases risk due to vascular constriction and damage |
|
Sedentary Lifestyle |
Contributes to obesity and hypertension, exacerbating angiopathy risk |
|
Diet High in Saturated Fats |
Promotes atherosclerosis and vascular disease |
Medical Conditions Associated with Angiopathy
Some medical conditions raise the risk of angiopathy. Diabetes, high blood pressure, and high cholesterol are big risks. Managing these conditions well is key to avoiding angiopathy problems.
Environmental Factors
Exposure to pollution and certain jobs can harm blood vessels. Avoiding these can lower the risk of getting angiopathy.
In short, angiopathy is caused by many things like genetics, lifestyle, health, and environment. Knowing and tackling these factors is key to preventing and managing angiopathic diseases.
Classification of Angiopathy: Macroangiopathy vs Microangiopathy
The size of the affected blood vessels is the key factor in distinguishing between the two main types of angiopathy.
Angiopathy is a term for vascular diseases. It is mainly split into macroangiopathy and microangiopathy based on the blood vessel size. Knowing these types is key for diagnosis and treatment.
Macroangiopathy: Large Vessel Disease
Macroangiopathy is about diseases in large blood vessels, like arteries and veins. It’s caused by plaque buildup or blood clots, reducing blood flow to important organs.
Characteristics of Macroangiopathy:
- Affects large arteries and veins
- Often linked to atherosclerosis
- Can cause heart attacks and strokes
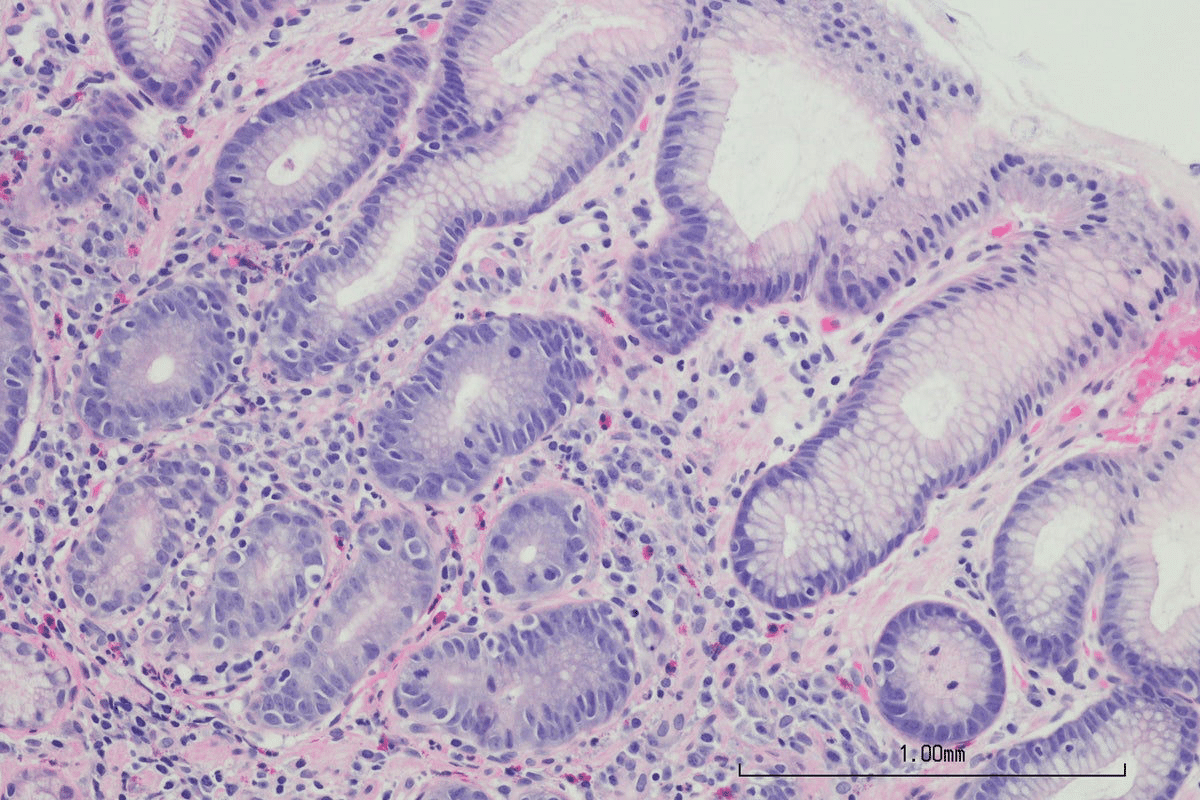
Microangiopathy: Small Vessel Disease
Microangiopathy deals with diseases in small blood vessels, like capillaries and small arteries. It’s marked by thickened vessel walls, which can block blood flow to tissues and organs.
Key Features of Microangiopathy:
- Affects small vessels, including capillaries
- Common in diabetes, causing retinopathy and nephropathy
- Can damage tissues due to poor blood supply
Macroangiopathy and microangiopathy have different effects on blood vessels.
|
Characteristics |
Macroangiopathy |
Microangiopathy |
|---|---|---|
|
Vessel Size |
Large vessels |
Small vessels |
|
Common Associations |
Atherosclerosis, cardiovascular events |
Diabetes, retinopathy, nephropathy |
|
Impact |
Reduced blood flow to organs, risk of heart attack and stroke |
Tissue damage, organ dysfunction |
It’s vital to know the differences between macroangiopathy and microangiopathy. This knowledge helps in creating effective treatments for vascular diseases.
Diabetic Angiopathy: The Most Prevalent Form
Diabetic angiopathy is a big problem for people with diabetes. It harms the blood vessels, causing heart issues. Knowing about diabetic angiopathy helps manage diabetes better.
Pathogenesis in Chronic Diabetes
Diabetic angiopathy starts with high blood sugar levels. High blood sugar damages the endothelium, causing inflammation and stress. This damage messes up blood vessel function, leading to angiopathic changes.
Endothelial Damage from Hyperglycemia
High blood sugar hurts the endothelium, a key part of blood vessels. Long-term high glucose levels harm endothelial function. It lowers nitric oxide and raises adhesion molecule levels.
Microvascular Complications
Microvascular problems are common in diabetic angiopathy. These include eye, kidney, and nerve damage. Damage from long-term high blood sugar and high blood pressure causes a lot of suffering.
Cardiovascular Mortality Statistics
Peripheral Angiopathy and Its Clinical Implications
It’s important to understand peripheral angiopathy to manage it well. This disease affects blood vessels outside the heart and brain. It can cause a lot of health problems and even death.
Symptoms and Clinical Presentation
The symptoms of peripheral angiopathy can differ based on how severe and where the disease is. Common signs include intermittent claudication, pain when not moving, and weak pulses. In bad cases, it can cause serious limb ischemia.
People with this disease may have mild or severe symptoms. Spotting these early is key to acting fast.
Diabetic Foot Ulcers: Development and Progression
Diabetic foot ulcers are a big problem for those with peripheral angiopathy, mainly in diabetics. These ulcers come from nerve damage, poor blood flow, and slow healing.
These ulcers can get worse fast, leading to amputation. So, it’s vital to prevent them and treat them early.
Amputation Risk Assessment and Prevention Strategies
It’s important to check if someone might lose a limb due to peripheral angiopathy. The risk goes up with disease severity, nerve damage, and past ulcers or amputations.
|
Risk Factor |
Description |
Prevention Strategy |
|---|---|---|
|
Peripheral Artery Disease |
Reduced blood flow to the limbs |
Revascularization procedures |
|
Diabetic Neuropathy |
Nerve damage leading to loss of sensation |
Regular foot examinations, patient education |
|
History of Ulcers or Amputations |
Previous history of foot ulcers or amputations |
Aggressive wound care, preventive foot care |
To prevent amputation, teach patients about foot care, check their feet often, and treat any foot problems quickly.
Cerebral Amyloid Angiopathy (CAA) and Neurological Impact
The buildup of amyloid-beta in brain vessel walls is key to CAA, a serious angiopathy. It affects the brain deeply. CAA happens when amyloid-beta peptides gather in small to medium-sized blood vessels in the brain. This causes many changes in the brain.
Pathological Features and Amyloid Deposition
CAA is known for amyloid-beta in vessel walls. This can make vessels thicker, more fragile, and prone to breaking. This buildup is linked to:
- Vascular inflammation
- Endothelial dysfunction
- Perivascular amyloid deposition
Clinical Manifestations and Neurological Symptoms
CAA symptoms can vary but often include:
- Cognitive decline
- Stroke, mainly lobar intracerebral hemorrhage
- Transient neurological symptoms
These symptoms come from the damage to blood vessels and amyloid buildup in CAA.
Relationship to Stroke and Cognitive Decline
CAA is a big risk for stroke and cognitive decline. The link between CAA and these issues is complex. It involves:
- Amyloid buildup making vessels fragile
- Higher chance of intracerebral hemorrhage
- Helping cause dementia through vascular and amyloid ways
It’s key to understand CAA’s role in these conditions to find better treatments.
Diagnosis and Assessment Methods for Angiopathic Conditions
Diagnosing angiopathy involves several steps. These include clinical checks, lab tests, and imaging. Getting the diagnosis right is key to treating the disease well.
Clinical Evaluation and Physical Examination
First, doctors take a detailed medical history and do a physical check. They look for signs like pain, numbness, or skin color changes. These can show if blood flow is blocked.
They also check pulses, blood pressure, and look for signs of poor blood flow. This helps them understand the situation better.
Laboratory Tests and Biomarkers
Lab tests are vital for diagnosing angiopathy. Tests like blood sugar, lipid levels, and inflammatory markers are common. They help spot problems early.
Biomarkers like HbA1c are key in diabetic angiopathy. They show how well blood sugar has been controlled over time.
Advanced Imaging Techniques
Imaging is key to seeing vascular damage. Angiography, ultrasound, and MRI give clear views of blood vessels. They help find blockages or damage.
These images guide treatment and track how the disease is progressing. They are very important.
Differential Diagnosis Considerations
When diagnosing angiopathy, it’s important to rule out other conditions. Symptoms can be similar to other diseases. Doctors must consider these to treat correctly.
A detailed diagnostic process helps find the right cause. This leads to better treatment plans for each patient.
In conclusion, diagnosing angiopathic conditions needs a complete approach. This includes clinical checks, lab tests, and imaging. Understanding these methods helps doctors create effective treatment plans for each patient.
Comprehensive Treatment Approaches for Angiopathy
Managing angiopathy well needs a mix of treatments. This condition harms blood vessels and affects their function. It requires many strategies to stop it from getting worse and to ease symptoms.
Medical Management and Pharmacotherapy
Medical care is key in treating angiopathic disease. Medicines play a big role in controlling symptoms and slowing the disease. Medications like antiplatelet agents, anticoagulants, and vasodilators are often used.
The right medicine depends on the cause and type of angiopathy. For example, in diabetic angiopathy, keeping blood sugar in check is vital to avoid more damage.
Surgical and Interventional Procedures
Sometimes, surgery or interventional methods are needed to fix blood flow issues. Angioplasty and stenting are common to open blocked or narrowed blood vessels.
For severe peripheral angiopathy, bypass surgery might be an option to improve blood flow. The choice to have surgery depends on how bad the symptoms are and if there are complications.
Lifestyle Modifications and Preventive Measures
Changing lifestyle is important in managing angiopathy and stopping it from getting worse. Stopping smoking, exercising regularly, and eating well are key parts of treatment.
People with angiopathy need to take care of their feet, even more so if they have diabetic foot ulcers. Keeping an eye on their feet and taking preventive steps can greatly lower the risk of losing a limb.
Emerging Therapies and Research Directions
Research on angiopathy is ongoing, with new treatments being explored. Gene therapy and regenerative medicine are being studied, holding promise for new treatments.
As we learn more about angiopathy’s molecular causes, we can develop targeted treatments. Clinical trials are important to check if these new treatments are safe and work well.
Conclusion: Living with and Managing Angiopathy
Managing angiopathy well is key to a better life for those with it. Knowing the causes, risks, and types helps patients manage their condition better.
Changing your lifestyle and getting medical help are important steps. Eating right and exercising can lower your risk of problems.
It’s important to keep up with care and check-ups. Following your treatment plan closely can slow the disease’s growth. Working with doctors helps create a plan for living with angiopathy.
Being proactive in managing angiopathy can greatly improve your health. It’s about a mix of medical care, lifestyle changes, and ongoing support.
FAQ
What is angiopathy?
Angiopathy is a disease that affects blood vessels. It comes from Greek words meaning “disease of blood vessels.”
What are the main types of angiopathy?
Angiopathy has two main types. Macroangiopathy affects big blood vessels. Microangiopathy affects small ones.
What is diabetic angiopathy?
Diabetic angiopathy happens in people with diabetes. High blood sugar damages blood vessels, causing problems.
What are the risk factors for developing angiopathy?
Risk factors include genetics and lifestyle choices like smoking. Medical conditions like diabetes and hypertension also play a role. Environmental factors matter too.
How is angiopathy diagnosed?
Doctors use clinical evaluation and lab tests to diagnose angiopathy. They also use imaging and differential diagnosis to find the cause.
What are the treatment approaches for angiopathy?
Treatment includes medical management and surgery. Lifestyle changes and new therapies are also used to manage the condition and prevent complications.
What is cerebral amyloid angiopathy (CAA)?
Cerebral amyloid angiopathy (CAA) is when amyloid protein builds up in brain blood vessels. It causes neurological symptoms and can lead to cognitive decline.
How does peripheral angiopathy affect the body?
Peripheral angiopathy can cause pain and numbness in limbs. It also raises the risk of diabetic foot ulcers and amputation.
Can angiopathy be prevented?
Some risk factors can’t be prevented. But, making lifestyle changes and managing medical conditions can lower the risk of getting angiopathy.
What is the impact of hyperglycemia on endothelial function?
High blood sugar damages the endothelium, the inner blood vessel lining. This leads to dysfunction and contributes to angiopathy.
What is the difference between macroangiopathy and microangiopathy?
Macroangiopathy affects large blood vessels. Microangiopathy affects small ones. They have different symptoms and complications.
Reference
World Health Organization. Angiopathy: Definition, Types, and Classification. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)























