Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.
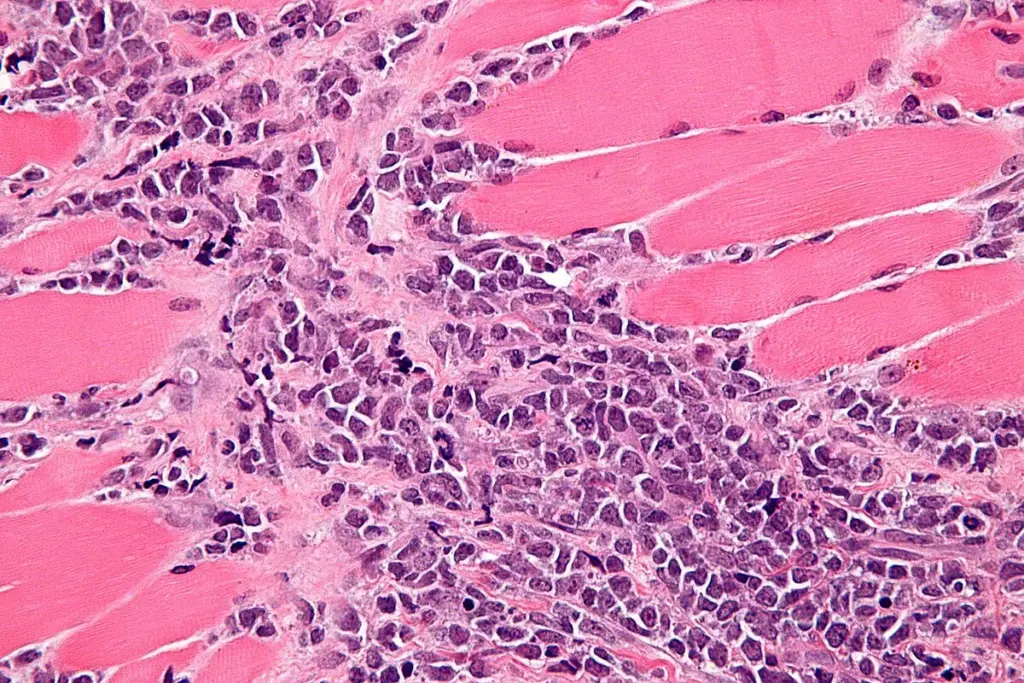
The therapeutic management of sarcoma is a paradigm of multidisciplinary oncology, requiring the coordinated expertise of orthopedic oncologists, surgical oncologists, medical oncologists, radiation oncologists, and pathologists. Because of the rarity and heterogeneity of the disease, treatment strategies are highly individualized and are dictated by histological subtype, grade, and anatomical location. The overarching goal is to achieve local control (removal of the tumor) while preventing systemic spread, maximizing functional preservation, and improving quality of life. The treatment landscape has evolved from amputation-based surgery to limb-salvage protocols integrated with precision radiation and molecularly targeted systemic therapies.
Surgical resection remains the cornerstone of curative treatment for localized sarcoma. The objective is a wide excision with negative margins, meaning a cuff of healthy tissue surrounds the removed tumor. In the extremities, this often involves Limb-Salvage Surgery. Instead of amputation, the surgeon removes the tumor and the involved bone or muscle, reconstructing the defect with metallic endoprostheses (artificial bone/joint replacements) or biological grafts. For soft-tissue sarcomas, this might require resection of major nerves or blood vessels, followed by complex microsurgical reconstruction to restore limb perfusion and function.
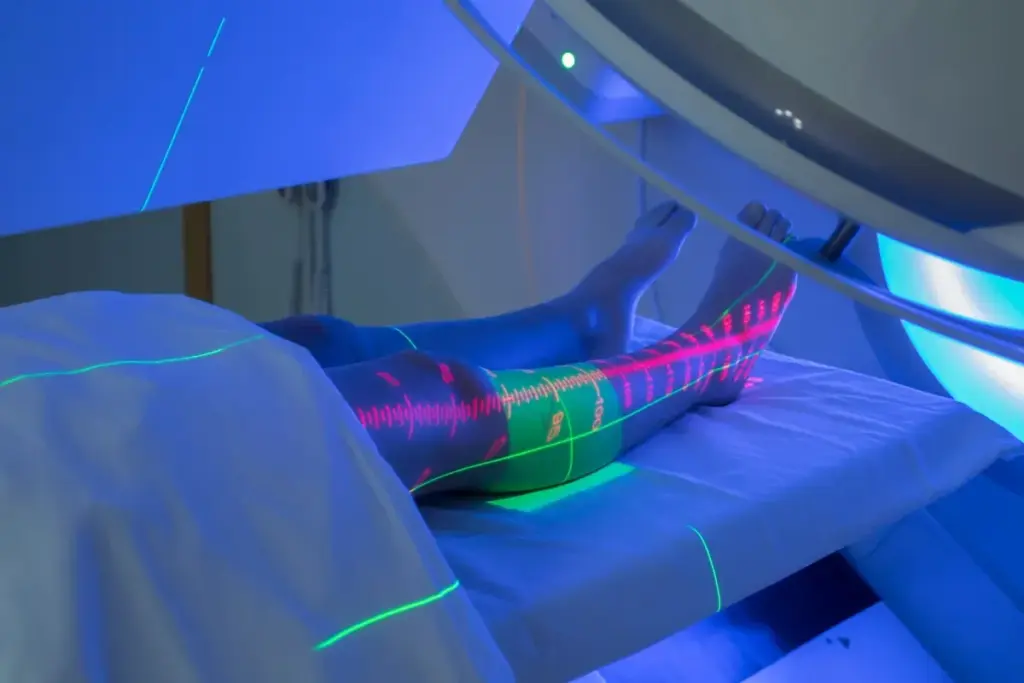
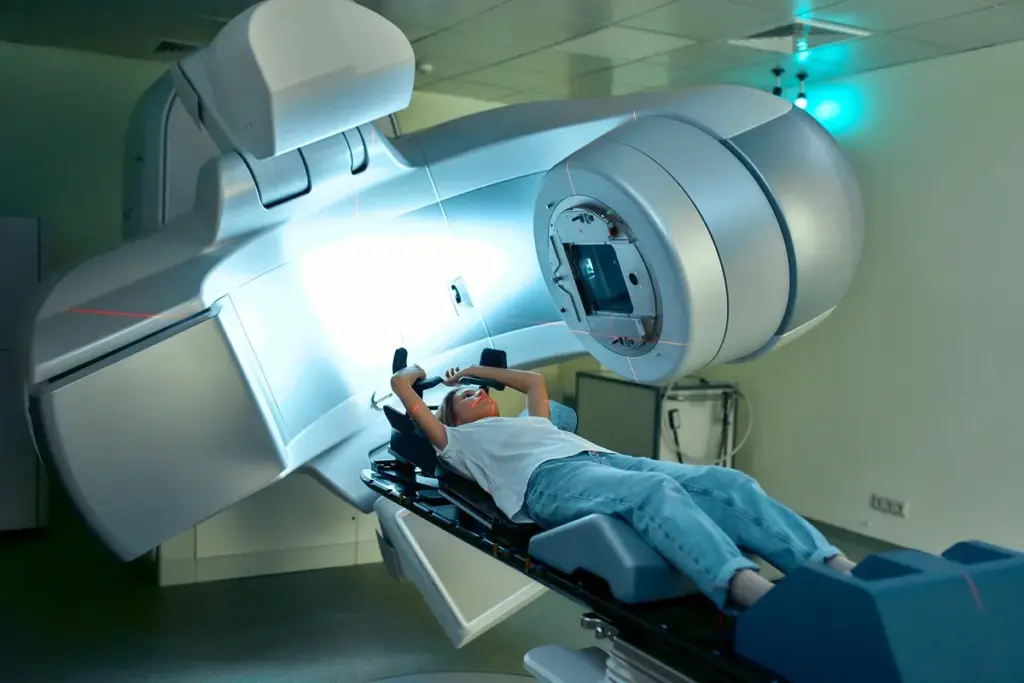
Radiation therapy is a critical adjunct to surgery, particularly for high-grade soft tissue sarcomas and those where wide surgical margins are difficult to achieve (e.g., near the spine or pelvis). It can be administered pre-operatively (neoadjuvant) or post-operatively (adjuvant). Neoadjuvant radiation has the advantage of shrinking the tumor, potentially making surgery easier, and the radiation field is smaller because the tissues haven’t been disturbed by surgery. However, it increases the risk of post-surgical wound healing complications. Adjuvant radiation avoids wound healing issues but requires a higher dose and a larger field to cover the surgical bed, potentially leading to more long-term fibrosis and joint stiffness. The choice depends on the specific tumor location and the patient’s healing capacity.
Chemotherapy is standard for chemosensitive bone sarcomas (Osteosarcoma, Ewing Sarcoma) and Rhabdomyosarcoma. The standard regimens often include Doxorubicin, Ifosfamide, Cisplatin, and Methotrexate. These are high-intensity protocols requiring inpatient admission. For adult soft tissue sarcomas, the role of chemotherapy is more nuanced and is typically reserved for high-grade tumors larger than 5 cm or for metastatic disease.
Targeted therapies have transformed the management of specific subtypes. Gastrointestinal Stromal Tumors (GIST) are the poster child for this approach; the use of Imatinib (Gleevec), a tyrosine kinase inhibitor targeting KIT/PDGFRA, has turned a fatal disease into a manageable chronic condition. Other targeted agents include Pazopanib (a multi-kinase inhibitor) for soft tissue sarcomas and Denosumab (a monoclonal antibody targeting RANK-ligand) for Giant Cell Tumor of Bone.
Immunotherapy with checkpoint inhibitors (PD-1/PD-L1 blockers) has shown promise in specific subtypes characterized by high mutational burden or viral etiology, such as Undifferentiated Pleomorphic Sarcoma and Kaposi Sarcoma. However, the dense, immunosuppressive extracellular matrix of many sarcomas limits the penetration of immune cells. Current research focuses on “priming” the tumor microenvironment—using radiation or intratumoral injections (such as oncolytic viruses like T-VEC) to turn a “cold” tumor “hot,” making it susceptible to systemic immunotherapy.

Metabolic targeting is an emerging frontier. Since sarcomas are highly dependent on specific nutrients like glutamine and arginine, drugs that deplete these amino acids or block their uptake are in clinical trials. For example, pegylated arginine deiminase (ADI-PEG20) starves arginine-auxotrophic sarcomas (such as leiomyosarcoma) of the arginine they cannot synthesize. This represents a shift towards exploiting the unique metabolic wiring of the mesenchymal cancer cell.

Send us all your questions or requests, and our expert team will assist you.
Limb-salvage surgery is a procedure to remove a bone or soft tissue tumor in an arm or leg without amputation. The surgeon removes the cancer and a margin of healthy tissue, then reconstructs the limb using a metal implant (prosthesis), a bone graft from another part of the body, or a donor bone. This preserves the appearance and function of the limb while effectively treating the cancer.
Pre-operative (neoadjuvant) radiation is often used to shrink the tumor, making it easier to remove and potentially allowing for a less invasive surgery that saves more function. It also creates a “rind” of dead tissue around the tumor, reducing the risk of live cancer cells being spilled during the operation.
Imatinib is a targeted therapy pill that revolutionized the treatment of Gastrointestinal Stromal Tumors (GIST). Unlike chemotherapy, which kills all fast-growing cells, Imatinib specifically blocks the abnormal proteins (KIT or PDGFRA) that tell the GIST cells to grow. It is highly effective and has fewer side effects than traditional chemotherapy.
Isolated Limb Perfusion is a specialized treatment for sarcomas confined to an arm or leg that cannot be removed surgically. The blood circulation of the limb is temporarily separated from the rest of the body, and high doses of chemotherapy are circulated only through that limb. This delivers a potent drug dose to the tumor without poisoning the rest of the body.
Immunotherapy is not yet a standard treatment for all sarcomas, but it shows promise for specific types. Checkpoint inhibitors (such as Pembrolizumab) can be effective for Undifferentiated Pleomorphic Sarcoma, Angiosarcoma, and other cancers. Clinical trials are ongoing to determine which patients benefit most from activating the immune system against mesenchymal tumors.

A bone cancer bone scan, also known as bone scintigraphy, is a test that uses a radioactive isotope. It finds areas of abnormal bone metabolism.

Bone scintigraphy is a detailed nuclear medicine imaging method. It helps find and diagnose different bone diseases. This includes fractures, infections, and cancer. A bone

Finding bone cancer early can really help patients. At Liv Hospital, we use the latest tech and care to help patients. Many tests help find


Finding bone cancer early is key to successful treatment, and at Liv Hospital we place the patient at the center of our care, using the

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)